

Volume 28, Issue 2 (Spring 2022)
Intern Med Today 2022, 28(2): 220-243 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rigi Kooteh B, Mojahed A, Sarani Yaztappeh J, Mousavi S E. Investigating the Effectiveness of Psychological Interventions (Mental-Educational) on the Quality of Sleep Among Patients With Chronic Diseases in Iran During 2003-2021: A Meta-Analytic Study. Intern Med Today 2022; 28 (2) :220-243
URL: http://imtj.gmu.ac.ir/article-1-3780-en.html
URL: http://imtj.gmu.ac.ir/article-1-3780-en.html
1- Department of Clinical Psychology, Children and Adolescents Health Research Center, Resistant Tuberculosis Institute, School of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran.
2- Department of Clinical Psychology, Health Promotion Research Center, Faculty of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran. ,mojahed@zaums.ac.ir
3- Department of Clinical Psychology, Faculty of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
2- Department of Clinical Psychology, Health Promotion Research Center, Faculty of Medicine, Zahedan University of Medical Sciences, Zahedan, Iran. ,
3- Department of Clinical Psychology, Faculty of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Keywords: Psychological Interventions, Quality of sleep, Patients with chronic disease, Meta-analysis
Full-Text [PDF 6913 kb]
(1355 Downloads)
| Abstract (HTML) (3409 Views)
Full-Text: (3853 Views)
Introduction
Sleep and rest are one of human needs causing cell repair and physical relaxation. Resting is considered a helper to the body’s function in growth, learning, and strengthening memory [1, 2]. Sleep disorders are considered one of the major public health problems that have a significant and negative impact on physical and social functioning as well as the quality of life [3]. Sleep and mental health are related to each other [4]. Poor quality of sleep is associated with depression [5], anxiety in cardiovascular patients [6], and increasing suicidal ideation. [7] Disruption of the sleep-wake cycle affects many of the body’s mental functions and leads to the feeling of fatigue, loss of concentration, psychiatric disorders, and premature death. [8] In addition, sleep disorders are associated with an increased risk of chronic diseases such as obesity, hypertension, type 2 diabetes, cancer, and depression. [9] Sleep disorders are highly prevalent in patients with type 2 diabetes in Iranian society which is also related to women’s age and gender [10].
Sleep-wake disorders are divided into two main groups including insomnia and sleep disorders. Sleep disorders include abnormal behavioral or physiological events that occur during sleep and include non-rapid eye movement sleep arousal disorder, nightmare disorder, rapid eye movement sleep disorder, restless legs syndrome, and sleep disorders caused by substances or drugs. People with insomnia cannot get enough sleep and are dissatisfied with the quality of their sleep, although they sleep all night, they do not feel refreshed, which include insomnia, hypersomnolence disorder, narcolepsy disorder, apnea disorders, and circadian rhythm disorders [11]. According to the importance of sleep disorders, many measures have been considered to reduce and prevent them. One of these ways is drug treatment. Different studies report different results regarding melatonin hypnotics on sleep disorders in patients with cancer. Melatonin consumption had a positive effect on comparisons of sleep quality, sleep duration, and sleep delay in patients with cancer. [12] On the other hand, some findings indicate that melatonin consumption for a week cannot improve insomnia in patients with cancer in stage four [13].
The use of pharmacotherapy and medications such as benzodiazepines, antidepressants, diphenhydramine, and antipsychotics reduces the delay in falling asleep or increases the duration of sleep; however, it leads to drug dependence and side effects such as drowsiness during the day, dizziness, mild headaches, ataxia, and memory impairment [13, 14, 16]. In addition to pharmacological methods, there are methods such as mental therapies that have different results. Mindfulness-based methods [17, 18], cognitive-behavioral therapy [19], dialectical behavior therapy [20], and group psychotherapy [21] are other methods to reduce sleep disorders. So far, several review and meta-analytical studies have been conducted to investigate the effect of psychological and non-pharmacological interventions on sleep disorders and sleep problems [22, 23, 24, 25, 26], the results of which show that psychological interventions are effective in reducing sleep problems.
In cognitive-behavioral therapy for insomnia, the elements of therapy include psychological education, cognitive therapy, behavioral strategies, and relaxation education; however, each of these elements can be presented separately. Cognitive-behavioral therapy with multiple elements is the preferred approach. Among these components is cognitive reconstruction, which is a sign of maladaptive thoughts and dysfunctional beliefs about sleep used to reduce sleep-related anxiety. Stimulus control includes limiting the behaviors that occur in the bedroom and ensuring that long periods of waking do not occur in bed. Also, restriction of sleep refers to the fact that it limits the time in bed, strengthens sleep, and increases sleep energy [27]. In mindfulness therapy, techniques are taught to clients to keep their attention on time, and anxiety is mainly considered and accepted instead of avoiding internal experiences. Therefore, mindfulness exercises increase the tolerance of clients’ anxiety, prevent avoidance that occurs as a habit, and improve and promote healthy mind-body function. It is possible that changing the relationship with cognitive contents and managing thought processes helps patients with insomnia and get them out of the cycle of thought rumination-arousal negative thoughts [28, 29].
A meta-analysis of 59 trials and 2102 patients with chronic insomnia showed that psychological interventions, on average, five hours after treatment, cause reliable changes in sleep delay and waking time after the onset of sleep. It is reduced by 30% with pharmacotherapy alone. Clinical improvements were maintained for six months at moderate follow-up. Stimulus control and sleep restriction were the most effective individual therapy methods, while sleep hygiene training was not effective when used alone [30]. Cognitive-behavioral therapy for insomnia is a combination of cognitive therapy, stimulus control therapy, and sleep restriction therapy with or without the use of relaxation therapy. Cognitive therapy involves consulting and writing the patient’s daily thoughts in a magazine or diary. It is possible that writing disturbing thoughts and worries before going to bed helps to transfer these thoughts on paper and clear the mind and make sleep easier. The goal is to change the patient’s misconceptions, beliefs, and attitudes that disturb sleep. There is not enough evidence to recommend cognitive therapy as a single method [15].
Studies on combination therapy show uncertain and variable results. Overall, these studies do not show a clear advantage for combination therapy compared to cognitive-behavioral therapy alone [31, 32]. In recent years, researchers have performed several group and individual interventions due to sleep problems in chronic physical patients in cost and time and compared the reduction of symptoms of sleep problems in the intervention subjects and the control group. However, experts still have different views on the effectiveness of this therapeutic approach. Accordingly, the theoretical knowledge obtained from conducting this research is more important than the findings of individual research due to the summary and integration of the results of various types of research helping theorists and therapists in the field of psychology to clarify the effectiveness of psychological interventions. Practically, if the effect of psychological interventions on the sleep quality of chronic physical patients is determined in this study, therapists can use it for people with more confidence and improve their performance. On the other hand, if it is possible to reach coherent conclusions based on this meta-analysis, this issue can make it needless for researchers to spend time and money on repetitive research in this field. Also, methodologically, although several studies have examined the effectiveness of this therapeutic approach on individual and group clients; so far, no coherent and comprehensive research has evaluated these studies by meta-analysis method. On the other hand, since there are huge studies on the effectiveness of psychological interventions on the sleep quality of chronic physical patients in Iran, it seems that performing a meta-analysis will help clarify the true value of the interventions and determine the effectiveness of these interventions. In other words, it is possible to achieve a more accurate and comprehensive view of the efficiency of the transcranial direct-current stimulation intervention model in the country by performing a meta-analysis. Accordingly, the present study intends to evaluate the effectiveness of psychological interventions on the quality of sleep in patients with chronic physical diseases using a meta-analysis study.
Materials and Methods
In the present study, the research method is meta-analysis based on the research goal. The concept of the meta-analysis was introduced by Glass in 1796. Meta-analysis is one of the methods that help to resolve contradictions in psychological research and other behavioral sciences and achieve more accurate results. Therefore, the combination meta-analysis of numerical results from several studies provides an accurate and complete estimate. Meta-analysis is a method that can be used to deduce the differences in the research and use them to achieve general and practical results [33]. A fundamental principle in meta-analysis studies is to calculate the effect size for separate studies and return them to a common general matrix and combine them to achieve the average effect. In meta-analysis, the effect size index related to r can be estimated with statistics such as T, F, and X [34].
The statistical population of the present study included all research, doctoral and master’s theses, and research published in domestic and international scientific journals which was conducted between 2003-2021 in the field of psychological interventions on the quality of sleep in patients with chronic physical diseases in Iran. The published studies had the necessary conditions in terms of methodology (hypothesis, research method, population, purpose, sample size, sampling method, measurement tool, validity and reliability of measuring tool, statistical analysis, and accuracy of statistical calculations). In total, 31 studies with 31 effect sizes were reviewed as study samples.
Instrument
Searching for studies in various sources is a significant issue in meta-analysis [34]. The sources of research in the present study were master’s and doctoral dissertations (referring researcher to the digital resources of the library and the university), scientific research journals in the field of psychology, educational sciences, medicine, Jihad Daneshgahi database, and the Iranian document centers. Sources were used and analyzed that examined the effect of psychological (mental-educational) interventions on the sleep quality of chronic physical patients in Iran as well as articles published by Iranian researchers in international journals. In the meta-analysis, all studies that have the required conditions in terms of methodology were analyzed. That is, all sources that had internal criteria have been used. In other words, the internal criteria for meta-analysis are:
(1) The research subject is psychological interventions and sleep quality in chronic physical patients; (2) The research is in the group, i.e. individual studies and review studies, but correlations are not acceptable for analysis; (3) Research is quasi-experimental; (4) Valid tools and accurate scales that have sufficient validity and credibility are used.
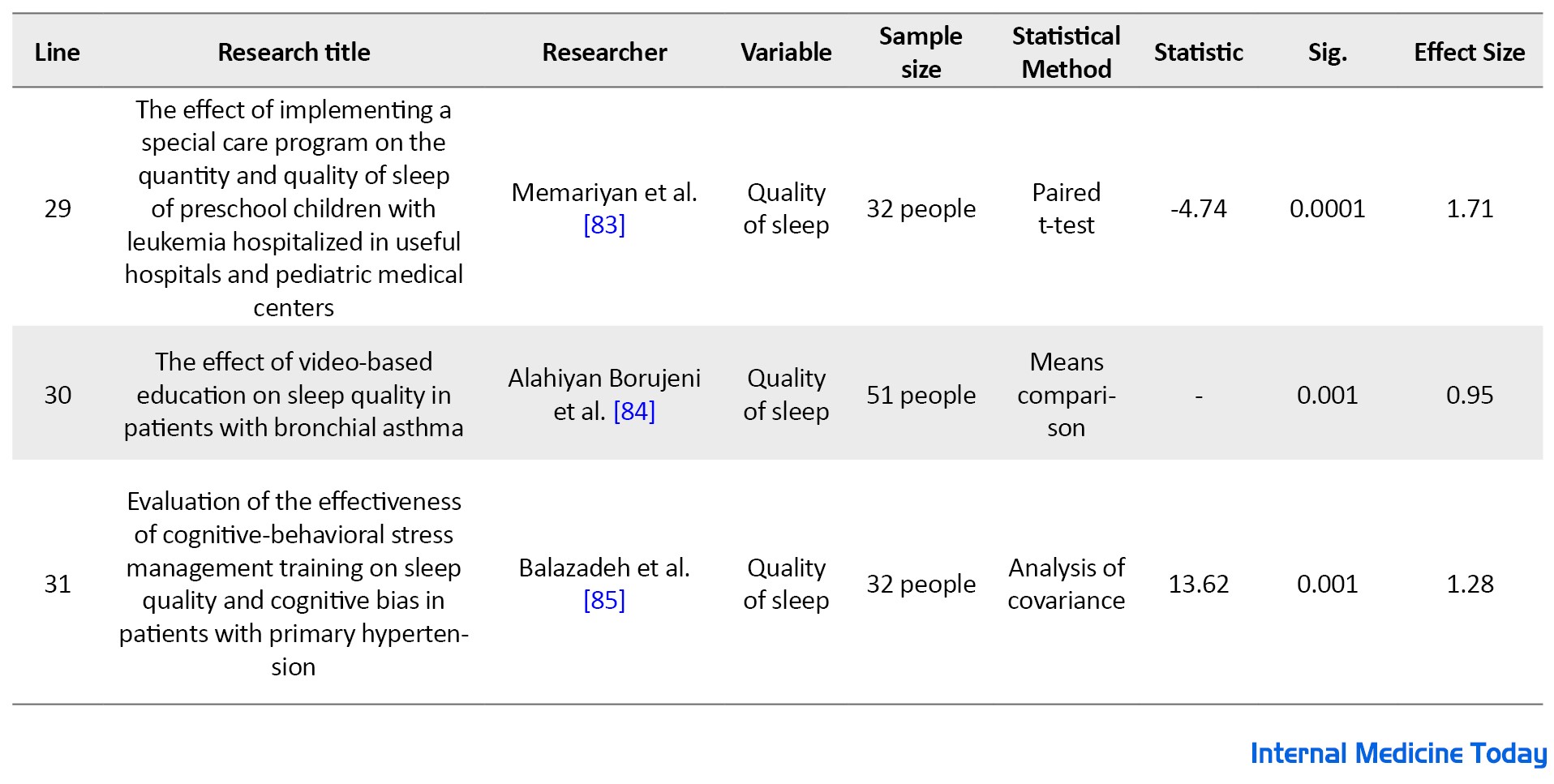
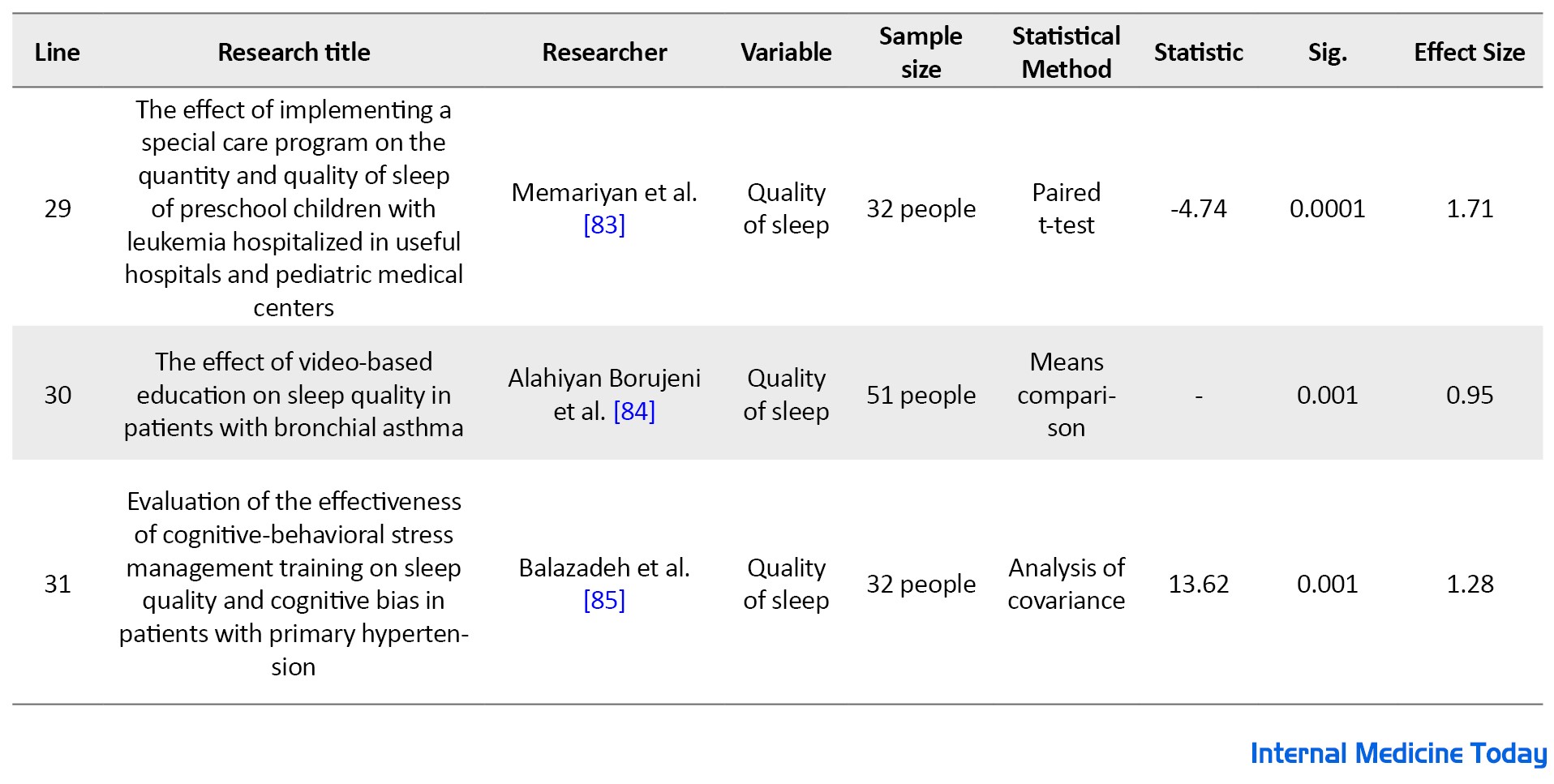
The tool used in this study was a content analysis checklist. This checklist was used to select dissertations, research projects, and research articles with criteria for entering and extracting the necessary information to perform a meta-analysis of their content. The checklist included the following components: Title of the research conducted, researcher name, variable, sample size, statistics used, statistics, and significance level. Meta-analysts can calculate the effect size by having the mean values, variance, standard deviation, and statistics used by the groups. However, the most common indices are r and d, in which d is used for group differences and r for correlation studies [35]. Therefore, according to the list of researches and referring to them and considering the mentioned criteria, 31 studies with 31 effect sizes were approved; the detailed list along with the descriptive information is presented in Table 1.
.jpg)
.jpg)
Calculations are done manually. The implementation stages of this meta-analysis are based on the meta-analysis of Howitt and Cramer (2005) [36] and are as follows as used in the present study:
(1) Definition of research variables; (2) Search databases; (3) Review of research; (4) Calculation of effect size for each study; (5) Combination of the effect size of studies; (6) Significance of combined studies. Table 1 shows the checklist of meta-analytical studies of psychological interventions (mental-educational) on the quality of sleep in patients with chronic physical diseases by the method of Howitt and Cramer (2005) in Iran (2003-2021).
Results
Of a total of 57 studies, 31 studies, including 1813 participants, had the eligibility criteria. Interventions included: follow-up care, massage therapy, progressive muscle relaxation, cognitive-behavioral group psychotherapy, mindfulness, Hatha Yoga, guided visualization, periodic exercise, sleep health education, foot massage, jaw relaxation, anger management group therapy, positive psychotherapy, special care program, cognitive-behavioral based stress management training, hope therapy, supportive intervention, cardiac rehabilitation, film training, and spiritual care. Groups of patients with chronic physical diseases include type 2 diabetes, multiple sclerosis, hemodialysis, breast cancer, chronic heart failure, coronary artery bypass grafting, obliterative bronchiolitis, myocardial infarction, leukemia, asthma, and hypertension.
In this section, according to the data provided in the report of each of the studies, the effect size of treatment patterns was calculated. For this purpose, the effect size was calculated according to the steps of the meta-analysis of Howitt and Cramer (2009), and all studies were then combined by converting each r of the effect to zr, calculating their average, and finally converting it to the volume of the effect. Table 2 shows the results of the meta-analysis of the effectiveness of psychological interventions (psychological-educational) on the sleep quality of chronic physical patients in Iran.
.jpg)
Table 2 shows the value of the significance level, z, r, d of Cohen and zr of Fisher for each study. The highest effect size is related to study 6 (Investigating the effect of Hatayoga exercises on sleep quality of hemodialysis patients, Haji Bala et al., (2014), with an effect size of 1.76 and a corrective effect of 0.793. The lowest reported effect size is related to study 25 (Investigating the effect of preferred music on sleep quality in patients undergoing coronary artery bypass surgery, Ghiasvandian et al., 2014) with an effect size of 0.02 and a corrective effect of 0.020.
The most important goal of a meta-analysis is to combine the findings of various studies as a unit volume of the composite effect. The method is to calculate the average volume of effects. Table 3 shows the composition of the results of the volume of the effects of examined studies.
.jpg)
According to the results obtained from Table 3, the average effect size obtained from the studies was equal to 0.99. Table 4 illustrates the significance of the combined studies.
.jpg)
According to the results obtained from Table 4, the combined significant level of the studies was P<0.00001, which indicates the significance of the total effect size of studies based on psychological interventions on the quality of sleep in patients with chronic physical diseases in Iran. Table 5 illustrates how to interpret the results based on Cohen’s d effect size.
.jpg)
The overall effect size of the present study is 0.99 which is high based on the results of Cohen’s d interpretation Table 5 which is significant (P<0.00001).
Discussion
Meta-analysis provides a more comprehensive view of the effect of different variables by integrating the results achieved by various studies performed on various samples. It examines a sample of a community and different people by collecting the results of research. Such findings are more important in communities such as the Iranian community, which is more diverse because this diversity is accompanied by more differences and inevitably, we need to obtain high information from different examples of this community to achieve similarities by integrating this information and deal with differences appropriately. In other words, the meta-analytic method allows the researcher to achieve more cognition of the phenomena by comparing the research with a method, because a general conclusion is obtained by combining the studies conducted [37].
It is significant to find and generalize the results of various studies in the field of psychological interventions on improving the quality of sleep in patients with chronic physical diseases as this study conducts. The present study estimated the effect size to be 0.99, which indicates a high effect size in Cohen’s interpretive evaluation that is significant. The results of this meta-analysis indicated that psychological interventions are effective treatments to improve sleep status in chronic physical patients in Iran. Therefore, the meta-analysis confirms the results of studies designed to evaluate the effectiveness of psychological interventions on the quality of sleep in patients with chronic physical diseases in Iran.
The results obtained in the present study are consistent with the studies achieved by Codsey, Bullock, Kennedy, and Tirley [38], Saruhanjan et al. [39], Moraski, Wade, Plotnikov, Lubans, and Duncan [40], Hansen, Huffling, Kruner-Bruevikov Stinger, and Style [41]. A meta-analysis of psychological interventions on sleep improvement in young adults was performed by Codsey, Bullock, Kennedy, and Tirley [38]. This systematic and review study was conducted to identify the effect size of randomized controlled trials of psychological interventions by reviewing 9 electronic databases. A total of 54 articles were selected for evaluation and 13 studies were suitable for meta-analysis based on the inclusion criteria. The combined effect size of all interventions was moderate indicating that the effectiveness of psychological interventions on sleep quality was significant in young adults.
Sarohanjan et al. [39] conducted a study entitled “The effectiveness of psychological interventions on sleep improvement in university students,” which was a meta-analytic study of controlled experimental studies. In this research, 10 studies were conducted with a randomized controlled trial with a sample of 2408 people. The overall average effect size for sleep quality from all study results indicates a moderate to high effect size for Cohen’s table. The effect size for sleep disorders was 0.79 and problems at the beginning of sleep were 0.65. Another study was conducted with the aim of the effectiveness of psychological therapies for chronic sleep nightmares by Hansen, Huffling, Kruner-Bruevikov Stinger, and Style [41]. The reported effect size for the study was 1.04, which indicates a high effect size.
A study was conducted by Moraski, Wade, Plutnikov, Lubans, and Duncan [40] with the aim of systematic evaluation and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Databases (age limit 18 to 64 years) and full text in English were examined. A total of 11 studies had the inclusion criteria. The results showed a moderate effect size. The intervention of stress management, relaxation, stimulus control, sleep hygiene, and exercise had the highest effect size.
According to the findings of the present study on the effect of psychological interventions on reducing sleep problems, psychological interventions including a multi-component cognitive-behavioral approach reduce cognitive arousal during sleep and reduce destructive sleep behaviors such as staying in bed [42]. This psychological approach affects false thoughts and beliefs, also, according to these psychological interventions, insomnia can be the result of inappropriate conditioning between environmental stimuli such as the bedroom and anti-sleep behaviors such as watching TV or reading in bed with restriction and sleep hygiene. It is specified that reconstructing or strengthening the relationship between sleep and stimuli is one of the methods of psychological intervention including the elimination of anti-sleep activities and the regulation of wake-sleep. Awareness of the sleep problem and correction of thoughts by not considering insomnia as a catastrophe, performing tasks with therapeutic properties and understanding cognitive errors, and breaking down the cognitive factors lead to the treatment [43, 44]. Also, sleep hygiene refers to the expansion of educating people about healthy lifestyle exercises that improve sleep [45]. Another therapeutic intervention is sleep therapy with conflicting intentions. In this intervention, the patient is advised to stay awake to reduce the anxiety caused by sleep pressure [46].
Conclusion
The results of the study conducted by Golafrooz et al. [47] indicated that self-care training according to the follow-up care model, which has four stages of identification, sensitization, control, and evaluation, leads to increased sleep quality in patients with type 2 diabetes. According to this model, for example, more than twenty effective factors on the quality of life prepared based on valid scientific texts are discussed and reviewed in the sensitization stage which can be a significant contributing factor to promote the health of people in the community.
Another therapeutic intervention for the quality of patients’ sleep is music therapy. Purposeful music therapy can help improve overall sleep quality and mental sleep quality and reduce the use of sleeping pills [48]. In this method, distracting the senses and reducing the focus on anxious environmental stimuli reduces the heart rate, anxiety, and depression and leads to pain relief [49]. Music can help improve the sleep quality of patients with acute and chronic sleep disorders. The music showed a cumulative dose effect for chronic sleep disorders and a follow-up period of more than three weeks is necessary to evaluate its effectiveness [50]. Progressive muscle relaxation is a technique in which a person feels relaxed through active contraction and then relaxation of specific muscle groups in a progressive state. In this method, muscle relaxation leads to peace of mind, reduces stress and anxiety, prevents the production of negative thoughts and emotions, and leads to increased sleep quality [51].
Massage therapy, as another psychological factor, improves sleep quality in patients [52]. In this method, the massage itself may create different levels of relaxation in the body of people under massage and therefore, it is possible to improve sleep quality at different levels [53, 54]. Also, spiritual care as a shield and protector to deal with physical and mental problems caused by chronic and severe diseases help people with an approach beyond normal life to achieve peace, relief from stress caused by illness, and quality of sleep [55]. Significantly, exercise and physical activity as non-pharmacological interventions improve sleep patterns having a positive effect on improving sleep quality by regulating central body temperature, melatonin secretion, and increasing growth hormone secretion [56].
Finally, paying attention to cultural contexts in different societies can be effective in the effectiveness of different treatment approaches. One of the distinctive features of meta-analysis is that the comparison of the effectiveness of different treatment models in different cultural contexts is possible to be provided. However the use of different therapeutic approaches in the treatment of problems is obvious, the success of the treatment model in solving the problem should be considered. Therefore, according to the results achieved by these studies, it is suggested that therapists use eclectic therapies or pharmacological therapies whose effectiveness has been proven to improve sleep quality in addition to psychological interventions. The lack of basic and coherent studies in the field of sleep disorders on the one hand, and the effectiveness of psychological interventions in reducing sleep disorders, on the other hand, has caused the need for additional studies, and the findings achieved by these studies to be felt and understood. The present study has been conducted to meet this need. However, more studies are needed on the effectiveness and continuity of the effects of psychological therapies with an emphasis on biological changes, and researchers need to examine these issues scientifically in a focused way. Moreover, it is suggested that further meta-analyses and review studies be conducted to determine whether there is a significant difference between pharmacotherapy or psychological interventions, and to what extent neuroscience techniques are effective in reducing sleep problems. The results of this meta-analysis for analysis of long-term impacts have limited generalizability because only 6 studies reported usable follow-up data during different periods. At the same time, since there is a high variety in the types of psychological interventions studied in the present meta-analysis, it is suggested that the general mechanisms of change be performed with a content analysis study or a review. Also, pharmacotherapy interventions are always at the forefront of reducing sleep problems, and it is better to conduct a study on the effectiveness of pharmacotherapy on the quality of sleep.
Ethical Considerations
Compliance with ethical guidelines
This article is a review study with no human or animal sample.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed equally in preparing all parts of the research
Conflicts of interest
The authors declared no conflict of interest.
References
Sleep and rest are one of human needs causing cell repair and physical relaxation. Resting is considered a helper to the body’s function in growth, learning, and strengthening memory [1, 2]. Sleep disorders are considered one of the major public health problems that have a significant and negative impact on physical and social functioning as well as the quality of life [3]. Sleep and mental health are related to each other [4]. Poor quality of sleep is associated with depression [5], anxiety in cardiovascular patients [6], and increasing suicidal ideation. [7] Disruption of the sleep-wake cycle affects many of the body’s mental functions and leads to the feeling of fatigue, loss of concentration, psychiatric disorders, and premature death. [8] In addition, sleep disorders are associated with an increased risk of chronic diseases such as obesity, hypertension, type 2 diabetes, cancer, and depression. [9] Sleep disorders are highly prevalent in patients with type 2 diabetes in Iranian society which is also related to women’s age and gender [10].
Sleep-wake disorders are divided into two main groups including insomnia and sleep disorders. Sleep disorders include abnormal behavioral or physiological events that occur during sleep and include non-rapid eye movement sleep arousal disorder, nightmare disorder, rapid eye movement sleep disorder, restless legs syndrome, and sleep disorders caused by substances or drugs. People with insomnia cannot get enough sleep and are dissatisfied with the quality of their sleep, although they sleep all night, they do not feel refreshed, which include insomnia, hypersomnolence disorder, narcolepsy disorder, apnea disorders, and circadian rhythm disorders [11]. According to the importance of sleep disorders, many measures have been considered to reduce and prevent them. One of these ways is drug treatment. Different studies report different results regarding melatonin hypnotics on sleep disorders in patients with cancer. Melatonin consumption had a positive effect on comparisons of sleep quality, sleep duration, and sleep delay in patients with cancer. [12] On the other hand, some findings indicate that melatonin consumption for a week cannot improve insomnia in patients with cancer in stage four [13].
The use of pharmacotherapy and medications such as benzodiazepines, antidepressants, diphenhydramine, and antipsychotics reduces the delay in falling asleep or increases the duration of sleep; however, it leads to drug dependence and side effects such as drowsiness during the day, dizziness, mild headaches, ataxia, and memory impairment [13, 14, 16]. In addition to pharmacological methods, there are methods such as mental therapies that have different results. Mindfulness-based methods [17, 18], cognitive-behavioral therapy [19], dialectical behavior therapy [20], and group psychotherapy [21] are other methods to reduce sleep disorders. So far, several review and meta-analytical studies have been conducted to investigate the effect of psychological and non-pharmacological interventions on sleep disorders and sleep problems [22, 23, 24, 25, 26], the results of which show that psychological interventions are effective in reducing sleep problems.
In cognitive-behavioral therapy for insomnia, the elements of therapy include psychological education, cognitive therapy, behavioral strategies, and relaxation education; however, each of these elements can be presented separately. Cognitive-behavioral therapy with multiple elements is the preferred approach. Among these components is cognitive reconstruction, which is a sign of maladaptive thoughts and dysfunctional beliefs about sleep used to reduce sleep-related anxiety. Stimulus control includes limiting the behaviors that occur in the bedroom and ensuring that long periods of waking do not occur in bed. Also, restriction of sleep refers to the fact that it limits the time in bed, strengthens sleep, and increases sleep energy [27]. In mindfulness therapy, techniques are taught to clients to keep their attention on time, and anxiety is mainly considered and accepted instead of avoiding internal experiences. Therefore, mindfulness exercises increase the tolerance of clients’ anxiety, prevent avoidance that occurs as a habit, and improve and promote healthy mind-body function. It is possible that changing the relationship with cognitive contents and managing thought processes helps patients with insomnia and get them out of the cycle of thought rumination-arousal negative thoughts [28, 29].
A meta-analysis of 59 trials and 2102 patients with chronic insomnia showed that psychological interventions, on average, five hours after treatment, cause reliable changes in sleep delay and waking time after the onset of sleep. It is reduced by 30% with pharmacotherapy alone. Clinical improvements were maintained for six months at moderate follow-up. Stimulus control and sleep restriction were the most effective individual therapy methods, while sleep hygiene training was not effective when used alone [30]. Cognitive-behavioral therapy for insomnia is a combination of cognitive therapy, stimulus control therapy, and sleep restriction therapy with or without the use of relaxation therapy. Cognitive therapy involves consulting and writing the patient’s daily thoughts in a magazine or diary. It is possible that writing disturbing thoughts and worries before going to bed helps to transfer these thoughts on paper and clear the mind and make sleep easier. The goal is to change the patient’s misconceptions, beliefs, and attitudes that disturb sleep. There is not enough evidence to recommend cognitive therapy as a single method [15].
Studies on combination therapy show uncertain and variable results. Overall, these studies do not show a clear advantage for combination therapy compared to cognitive-behavioral therapy alone [31, 32]. In recent years, researchers have performed several group and individual interventions due to sleep problems in chronic physical patients in cost and time and compared the reduction of symptoms of sleep problems in the intervention subjects and the control group. However, experts still have different views on the effectiveness of this therapeutic approach. Accordingly, the theoretical knowledge obtained from conducting this research is more important than the findings of individual research due to the summary and integration of the results of various types of research helping theorists and therapists in the field of psychology to clarify the effectiveness of psychological interventions. Practically, if the effect of psychological interventions on the sleep quality of chronic physical patients is determined in this study, therapists can use it for people with more confidence and improve their performance. On the other hand, if it is possible to reach coherent conclusions based on this meta-analysis, this issue can make it needless for researchers to spend time and money on repetitive research in this field. Also, methodologically, although several studies have examined the effectiveness of this therapeutic approach on individual and group clients; so far, no coherent and comprehensive research has evaluated these studies by meta-analysis method. On the other hand, since there are huge studies on the effectiveness of psychological interventions on the sleep quality of chronic physical patients in Iran, it seems that performing a meta-analysis will help clarify the true value of the interventions and determine the effectiveness of these interventions. In other words, it is possible to achieve a more accurate and comprehensive view of the efficiency of the transcranial direct-current stimulation intervention model in the country by performing a meta-analysis. Accordingly, the present study intends to evaluate the effectiveness of psychological interventions on the quality of sleep in patients with chronic physical diseases using a meta-analysis study.
Materials and Methods
In the present study, the research method is meta-analysis based on the research goal. The concept of the meta-analysis was introduced by Glass in 1796. Meta-analysis is one of the methods that help to resolve contradictions in psychological research and other behavioral sciences and achieve more accurate results. Therefore, the combination meta-analysis of numerical results from several studies provides an accurate and complete estimate. Meta-analysis is a method that can be used to deduce the differences in the research and use them to achieve general and practical results [33]. A fundamental principle in meta-analysis studies is to calculate the effect size for separate studies and return them to a common general matrix and combine them to achieve the average effect. In meta-analysis, the effect size index related to r can be estimated with statistics such as T, F, and X [34].
The statistical population of the present study included all research, doctoral and master’s theses, and research published in domestic and international scientific journals which was conducted between 2003-2021 in the field of psychological interventions on the quality of sleep in patients with chronic physical diseases in Iran. The published studies had the necessary conditions in terms of methodology (hypothesis, research method, population, purpose, sample size, sampling method, measurement tool, validity and reliability of measuring tool, statistical analysis, and accuracy of statistical calculations). In total, 31 studies with 31 effect sizes were reviewed as study samples.
Instrument
Searching for studies in various sources is a significant issue in meta-analysis [34]. The sources of research in the present study were master’s and doctoral dissertations (referring researcher to the digital resources of the library and the university), scientific research journals in the field of psychology, educational sciences, medicine, Jihad Daneshgahi database, and the Iranian document centers. Sources were used and analyzed that examined the effect of psychological (mental-educational) interventions on the sleep quality of chronic physical patients in Iran as well as articles published by Iranian researchers in international journals. In the meta-analysis, all studies that have the required conditions in terms of methodology were analyzed. That is, all sources that had internal criteria have been used. In other words, the internal criteria for meta-analysis are:
(1) The research subject is psychological interventions and sleep quality in chronic physical patients; (2) The research is in the group, i.e. individual studies and review studies, but correlations are not acceptable for analysis; (3) Research is quasi-experimental; (4) Valid tools and accurate scales that have sufficient validity and credibility are used.
The tool used in this study was a content analysis checklist. This checklist was used to select dissertations, research projects, and research articles with criteria for entering and extracting the necessary information to perform a meta-analysis of their content. The checklist included the following components: Title of the research conducted, researcher name, variable, sample size, statistics used, statistics, and significance level. Meta-analysts can calculate the effect size by having the mean values, variance, standard deviation, and statistics used by the groups. However, the most common indices are r and d, in which d is used for group differences and r for correlation studies [35]. Therefore, according to the list of researches and referring to them and considering the mentioned criteria, 31 studies with 31 effect sizes were approved; the detailed list along with the descriptive information is presented in Table 1.
.jpg)
.jpg)
Calculations are done manually. The implementation stages of this meta-analysis are based on the meta-analysis of Howitt and Cramer (2005) [36] and are as follows as used in the present study:
(1) Definition of research variables; (2) Search databases; (3) Review of research; (4) Calculation of effect size for each study; (5) Combination of the effect size of studies; (6) Significance of combined studies. Table 1 shows the checklist of meta-analytical studies of psychological interventions (mental-educational) on the quality of sleep in patients with chronic physical diseases by the method of Howitt and Cramer (2005) in Iran (2003-2021).
Results
Of a total of 57 studies, 31 studies, including 1813 participants, had the eligibility criteria. Interventions included: follow-up care, massage therapy, progressive muscle relaxation, cognitive-behavioral group psychotherapy, mindfulness, Hatha Yoga, guided visualization, periodic exercise, sleep health education, foot massage, jaw relaxation, anger management group therapy, positive psychotherapy, special care program, cognitive-behavioral based stress management training, hope therapy, supportive intervention, cardiac rehabilitation, film training, and spiritual care. Groups of patients with chronic physical diseases include type 2 diabetes, multiple sclerosis, hemodialysis, breast cancer, chronic heart failure, coronary artery bypass grafting, obliterative bronchiolitis, myocardial infarction, leukemia, asthma, and hypertension.
In this section, according to the data provided in the report of each of the studies, the effect size of treatment patterns was calculated. For this purpose, the effect size was calculated according to the steps of the meta-analysis of Howitt and Cramer (2009), and all studies were then combined by converting each r of the effect to zr, calculating their average, and finally converting it to the volume of the effect. Table 2 shows the results of the meta-analysis of the effectiveness of psychological interventions (psychological-educational) on the sleep quality of chronic physical patients in Iran.
.jpg)
Table 2 shows the value of the significance level, z, r, d of Cohen and zr of Fisher for each study. The highest effect size is related to study 6 (Investigating the effect of Hatayoga exercises on sleep quality of hemodialysis patients, Haji Bala et al., (2014), with an effect size of 1.76 and a corrective effect of 0.793. The lowest reported effect size is related to study 25 (Investigating the effect of preferred music on sleep quality in patients undergoing coronary artery bypass surgery, Ghiasvandian et al., 2014) with an effect size of 0.02 and a corrective effect of 0.020.
The most important goal of a meta-analysis is to combine the findings of various studies as a unit volume of the composite effect. The method is to calculate the average volume of effects. Table 3 shows the composition of the results of the volume of the effects of examined studies.
.jpg)
According to the results obtained from Table 3, the average effect size obtained from the studies was equal to 0.99. Table 4 illustrates the significance of the combined studies.
.jpg)
According to the results obtained from Table 4, the combined significant level of the studies was P<0.00001, which indicates the significance of the total effect size of studies based on psychological interventions on the quality of sleep in patients with chronic physical diseases in Iran. Table 5 illustrates how to interpret the results based on Cohen’s d effect size.
.jpg)
The overall effect size of the present study is 0.99 which is high based on the results of Cohen’s d interpretation Table 5 which is significant (P<0.00001).
Discussion
Meta-analysis provides a more comprehensive view of the effect of different variables by integrating the results achieved by various studies performed on various samples. It examines a sample of a community and different people by collecting the results of research. Such findings are more important in communities such as the Iranian community, which is more diverse because this diversity is accompanied by more differences and inevitably, we need to obtain high information from different examples of this community to achieve similarities by integrating this information and deal with differences appropriately. In other words, the meta-analytic method allows the researcher to achieve more cognition of the phenomena by comparing the research with a method, because a general conclusion is obtained by combining the studies conducted [37].
It is significant to find and generalize the results of various studies in the field of psychological interventions on improving the quality of sleep in patients with chronic physical diseases as this study conducts. The present study estimated the effect size to be 0.99, which indicates a high effect size in Cohen’s interpretive evaluation that is significant. The results of this meta-analysis indicated that psychological interventions are effective treatments to improve sleep status in chronic physical patients in Iran. Therefore, the meta-analysis confirms the results of studies designed to evaluate the effectiveness of psychological interventions on the quality of sleep in patients with chronic physical diseases in Iran.
The results obtained in the present study are consistent with the studies achieved by Codsey, Bullock, Kennedy, and Tirley [38], Saruhanjan et al. [39], Moraski, Wade, Plotnikov, Lubans, and Duncan [40], Hansen, Huffling, Kruner-Bruevikov Stinger, and Style [41]. A meta-analysis of psychological interventions on sleep improvement in young adults was performed by Codsey, Bullock, Kennedy, and Tirley [38]. This systematic and review study was conducted to identify the effect size of randomized controlled trials of psychological interventions by reviewing 9 electronic databases. A total of 54 articles were selected for evaluation and 13 studies were suitable for meta-analysis based on the inclusion criteria. The combined effect size of all interventions was moderate indicating that the effectiveness of psychological interventions on sleep quality was significant in young adults.
Sarohanjan et al. [39] conducted a study entitled “The effectiveness of psychological interventions on sleep improvement in university students,” which was a meta-analytic study of controlled experimental studies. In this research, 10 studies were conducted with a randomized controlled trial with a sample of 2408 people. The overall average effect size for sleep quality from all study results indicates a moderate to high effect size for Cohen’s table. The effect size for sleep disorders was 0.79 and problems at the beginning of sleep were 0.65. Another study was conducted with the aim of the effectiveness of psychological therapies for chronic sleep nightmares by Hansen, Huffling, Kruner-Bruevikov Stinger, and Style [41]. The reported effect size for the study was 1.04, which indicates a high effect size.
A study was conducted by Moraski, Wade, Plutnikov, Lubans, and Duncan [40] with the aim of systematic evaluation and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Databases (age limit 18 to 64 years) and full text in English were examined. A total of 11 studies had the inclusion criteria. The results showed a moderate effect size. The intervention of stress management, relaxation, stimulus control, sleep hygiene, and exercise had the highest effect size.
According to the findings of the present study on the effect of psychological interventions on reducing sleep problems, psychological interventions including a multi-component cognitive-behavioral approach reduce cognitive arousal during sleep and reduce destructive sleep behaviors such as staying in bed [42]. This psychological approach affects false thoughts and beliefs, also, according to these psychological interventions, insomnia can be the result of inappropriate conditioning between environmental stimuli such as the bedroom and anti-sleep behaviors such as watching TV or reading in bed with restriction and sleep hygiene. It is specified that reconstructing or strengthening the relationship between sleep and stimuli is one of the methods of psychological intervention including the elimination of anti-sleep activities and the regulation of wake-sleep. Awareness of the sleep problem and correction of thoughts by not considering insomnia as a catastrophe, performing tasks with therapeutic properties and understanding cognitive errors, and breaking down the cognitive factors lead to the treatment [43, 44]. Also, sleep hygiene refers to the expansion of educating people about healthy lifestyle exercises that improve sleep [45]. Another therapeutic intervention is sleep therapy with conflicting intentions. In this intervention, the patient is advised to stay awake to reduce the anxiety caused by sleep pressure [46].
Conclusion
The results of the study conducted by Golafrooz et al. [47] indicated that self-care training according to the follow-up care model, which has four stages of identification, sensitization, control, and evaluation, leads to increased sleep quality in patients with type 2 diabetes. According to this model, for example, more than twenty effective factors on the quality of life prepared based on valid scientific texts are discussed and reviewed in the sensitization stage which can be a significant contributing factor to promote the health of people in the community.
Another therapeutic intervention for the quality of patients’ sleep is music therapy. Purposeful music therapy can help improve overall sleep quality and mental sleep quality and reduce the use of sleeping pills [48]. In this method, distracting the senses and reducing the focus on anxious environmental stimuli reduces the heart rate, anxiety, and depression and leads to pain relief [49]. Music can help improve the sleep quality of patients with acute and chronic sleep disorders. The music showed a cumulative dose effect for chronic sleep disorders and a follow-up period of more than three weeks is necessary to evaluate its effectiveness [50]. Progressive muscle relaxation is a technique in which a person feels relaxed through active contraction and then relaxation of specific muscle groups in a progressive state. In this method, muscle relaxation leads to peace of mind, reduces stress and anxiety, prevents the production of negative thoughts and emotions, and leads to increased sleep quality [51].
Massage therapy, as another psychological factor, improves sleep quality in patients [52]. In this method, the massage itself may create different levels of relaxation in the body of people under massage and therefore, it is possible to improve sleep quality at different levels [53, 54]. Also, spiritual care as a shield and protector to deal with physical and mental problems caused by chronic and severe diseases help people with an approach beyond normal life to achieve peace, relief from stress caused by illness, and quality of sleep [55]. Significantly, exercise and physical activity as non-pharmacological interventions improve sleep patterns having a positive effect on improving sleep quality by regulating central body temperature, melatonin secretion, and increasing growth hormone secretion [56].
Finally, paying attention to cultural contexts in different societies can be effective in the effectiveness of different treatment approaches. One of the distinctive features of meta-analysis is that the comparison of the effectiveness of different treatment models in different cultural contexts is possible to be provided. However the use of different therapeutic approaches in the treatment of problems is obvious, the success of the treatment model in solving the problem should be considered. Therefore, according to the results achieved by these studies, it is suggested that therapists use eclectic therapies or pharmacological therapies whose effectiveness has been proven to improve sleep quality in addition to psychological interventions. The lack of basic and coherent studies in the field of sleep disorders on the one hand, and the effectiveness of psychological interventions in reducing sleep disorders, on the other hand, has caused the need for additional studies, and the findings achieved by these studies to be felt and understood. The present study has been conducted to meet this need. However, more studies are needed on the effectiveness and continuity of the effects of psychological therapies with an emphasis on biological changes, and researchers need to examine these issues scientifically in a focused way. Moreover, it is suggested that further meta-analyses and review studies be conducted to determine whether there is a significant difference between pharmacotherapy or psychological interventions, and to what extent neuroscience techniques are effective in reducing sleep problems. The results of this meta-analysis for analysis of long-term impacts have limited generalizability because only 6 studies reported usable follow-up data during different periods. At the same time, since there is a high variety in the types of psychological interventions studied in the present meta-analysis, it is suggested that the general mechanisms of change be performed with a content analysis study or a review. Also, pharmacotherapy interventions are always at the forefront of reducing sleep problems, and it is better to conduct a study on the effectiveness of pharmacotherapy on the quality of sleep.
Ethical Considerations
Compliance with ethical guidelines
This article is a review study with no human or animal sample.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed equally in preparing all parts of the research
Conflicts of interest
The authors declared no conflict of interest.
References
- Bozorg Sohrabi F, Soleymani A, Habibi MR, Emami zeydi A, Nejad Gorji HS, Hasanzade kiab F. [Sleep quality and its related factors in nurses, work in open heart intensive care Units in Mazandaran providence: A cross-sectional study (Persian)]. Journal of Health Breeze. 2014; 2(1):18-23. [Link]
- Mohammadian M, Khosravi A, Nohi S, Mousavi SA. [Factor associated with self-reported sleep quality in adults-a population based study (Persian)]. Knowledge and Health. 2018; 12(4):1-6. [Link]
- Redline S, Foody J. Sleep disturbances: Time to join the top 10 potentially modifiable cardiovascular risk factors? Circulation. 2011; 124(19):2049-51. [PMID]
- Zou P, Wang X, Sun L, Liu K, Hou G, Yang W, et al. Poorer sleep quality correlated with mental health problems in college students: A longitudinal observational study among 686 males. Journal of Psychosomatic Research. 2020, 136:110177. [PMID]
- Liu X, Wang C, Qiao X, Si H, Jin Y. Sleep quality, depression and frailty among Chinese community-dwelling older adults. Geriatric Nursing. 2021, 42(3):714-20. [DOI:10.1016/j.gerinurse.2021.02.020] [PMID]
- Matsuda R, Kohno T, Kohsaka S, Fukuoka R, Maekawa Y, Sano M, et al. The prevalence of poor sleep quality and its association with depression and anxiety scores in patients admitted for cardiovascular disease: A cross-sectional designed study. International Journal of Cardiology. 2017; 228:977-82. [PMID]
- Shi X, Xu L, Wang Z, Wang Sh, Wang A, Hu X, et al. Poor sleep quality and suicidal ideation among Chinese community adults: A moderated mediation model of mental distress and family functioning. Current Psychology. 2021; 1-12. [DOI:10.1007/s12144-021-01845-x]
- Serin Y, Acar Tek N. Effect of circadian rhythm on metabolic processes and the regulation of energy balance. Annals of Nutrition & Metabolism. 2019; 74(4):322-30. [PMID]
- Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep disorders and sleep deprivation: An unmet public health problem. Washington (DC): National Academies Press; 2006. [PMID]
- Khorasani ZM, Ravan VR, Hejazi S. Evaluation of the prevalence of sleep disorder among patients with type 2 diabetes mellitus referring to Ghaem Hospital from 2016 to 2017. Current Diabetes Reviews. 2021; 17(2):214-21. [PMID]
- Arlington: American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Virginia: American Psychiatric Association; 2013. [DOI:10.1176/appi.books.9780890425596]
- Farshchian N, Shirzadi M, Farshchian F, Tanhaye S, Heydarheydari S, Amirifard N. [Evaluation of the melatonin effect on sleep quality in cancer patients (Persian)]. Tehran University Medical Journal. 2020; 78(1):38-42. [Link]
- Farahbakhsh A, Dehghani F. [Effectiveness of Mindfulness therapy in sleep quality and mental health of women with insomnia disorder (Persian)]. Journal of Torbat Heydariyeh University of Medical Sciences. 2016; 4(3):8-15. [Link]
- Tsai JH, Yang P, Chen CC, Chung W, Tang TC, Wang SY, et al. Zolpidem-induced amnesia and somnambulism: Rare occurrences? European Neuropsychopharmacology. 2009; 19(1):74-6. [PMID]
- Morgenthaler T, Kramer M, Alessi C, Friedman L, Boehlecke B, Kapur V, et al. Practice parameters for the psychological and behavioral treatment of insomnia: An update. An American Academy of Sleep Medicine Report. 2006, 29(11):1415-9. [DOI:10.1093/sleep/29.11.1415]
- Han KH, Kim SY, Chung SY. Effect of acupuncture on patients with insomnia: Study protocols for a randomized controlled trial. Trials. 2014; 15:403. [PMID] [PMCID]
- Rusch HL, Rosario M, Levison LM, Olivera A, Livingston WS, Wu T, et al. The effect of mindfulness meditation on sleep quality: A systematic review and meta-analysis of randomized controlled trials. Annals of the New York Academy of Sciences. 2019; 1445(1):5-16. [PMID] [PMCID]
- Jones BJ, Kaur S, Miller M, Spencer RMC. Mindfulness-based stress reduction benefits psychological well-being, sleep quality, and athletic performance in female collegiate rowers. Frontiers in Psychology. 2020; 11:572980 [PMID] [PMCID]
- Perfect MM, Elkins GR. Cognitive-behavioral therapy and hypnotic relaxation to treat sleep problems in an adolescent with diabetes. Journal of Clinical Psychology. 2010; 66(11):1205-15. [DOI:10.1002/jclp.20732] [PMID] [PMCID]
- Mohamadi J, Gholamrezae S, Azizi A. [Effectiveness of dialectical behavior therapy on quality ofsleep and anxiety in patients with irritable bowel syndrome (Persian)]. Iranian Journal of Psychiatric Nursing. 2015; 3(2):21-30. [Link]
- Mao H, Ji Y, Xu Y, Tang G, Yu Z, Xu L, et al. Group cognitive-behavioral therapy in insomnia: A cross-sectional case-controlled study. Neuropsychiatric Disease and Treatment. 2017; 13:2841-8. [PMID] [PMCID]
- Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Ghasemi H, Mohammadi M, et al. The effect of acceptance and commitment therapy on insomnia and sleep quality: A systematic review. BMC Neurology. 2020; 20(1):300. [PMID] [PMCID]
- Papaconstantinou E, Cancelliere C, Verville L, Wong JJ, Connell G, Yu H, et al. Effectiveness of non-pharmacological interventions on sleep characteristics among adults with musculoskeletal pain and a comorbid sleep problem: A systematic review. Chiropractic & Manual Therapies. 2021; 29(1):23. [DOI:10.1186/s12998-021-00381-6] [PMID] [PMCID]
- Mitchell LJ, Bisdounis L, Ballesio A, Omlin X, Kyle SD. The impact of cognitive behavioural therapy for insomnia on objective sleep parameters: A meta-analysis and systematic review. Sleep Medicine Reviews. 2019; 47:90-102. [DOI:10.1016/j.smrv.2019.06.002] [PMID]
- Trauer JM, Qian MY, Doyle JS, Rajaratnam SM, Cunnington D. Cognitive behavioral therapy for chronic insomnia: A systematic review and meta-analysis. Annals of Internal Medicine. 2015; 163(3):191-204. [DOI:10.7326/M14-2841] [PMID]
- Wu JQ, Appleman ER, Salazar RD, Ong JC. Cognitive behavioral therapy for insomnia comorbid with psychiatric and medical conditions: A meta-analysis. JAMA Internal Medicine. 2015; 175(9):1461-72. [DOI:10.1001/jamainternmed.2015.3006] [PMID]
- Koffel EA, Koffel JB, Gehrman PR. A meta-analysis of group cognitive behavioral therapy for insomnia. Sleep Medicine Reviews. 2015; 19:6-16. [PMID] [PMCID]
- Greeson J, Brantley J. Mindfulness and anxiety disorders: Developing a wise relationship with the inner experience of fear. In: Didonna F, editor. Clinical handbook of mindfulness. New York: Springer; 2009. [DOI:10.1007/978-0-387-09593-6_11]
- Semple R, Lee J. Treating anxiety with mindfulness: Mindfulness-based cognitive therapy for children. In: Laurie A. Greco, Steven C. Hayes, editors. Acceptance and mindfulness interventions for children, adolescents, and families: A practitioner’s guide. California: New Harbinger; 2008. [Link]
- Morin CM, Culbert JP, Schwartz SM. Nonpharmacological interventions for insomnia: A meta-analysis of treatment efficacy. The American Journal of Psychiatry. 1994, 151(8):1172-80. [DOI:10.1176/ajp.151.8.1172] [PMID]
- Hauri PJ. Can we mix behavioral therapy with hypnotics when treating insomniacs? Sleep. 1997; 20(12):1111-8. [DOI:10.1093/sleep/20.12.1111] [PMID]
- Morin CM, Colecchi C, Stone J, Sood R, Brink D. Behavioral and pharmacological therapies for late-life insomnia: A randomized controlled trial. JAMA. 1999; 281(11):991-9. [DOI:10.1001/jama.281.11.991] [PMID]
- Ezanloo B, Habibi M. [Application of meta-analysis in social and behavioral science: A review of advantages, disadvantages, and methodological issues (Persian)]. Journal of Research in Behavioural Sciences. 2011; 9(1):70-82. [Link]
- Farahani H, Oreyzi H. [Advanced methods in humanities (Persian)]. Isfahan: Jahade-Daneshgahi; 2005. [Link]
- Delavar A. [Theoretical and practical principles of research in the humanities and social sciences (Persian)]. Tehran: Roshd; 2020. [Link]
- Howitt D, Cramer, D. Introduction to SPSS in psychology [H. Pasha Sharifi, J. Najafizadeh, M. Mirhashemi, D. Manavipour, N. Sharifi, Persian trans]. Tehran: Sokhan; 2010. [Link]
- Rashidi A, Faramarzi S, Shamsi A. [Meta-analysis of the effect of psychological nervous interventions on improving academic performance in students with specific learning disabilities (Persian)]. Shenakht Journal of Psychology and Psychiatry. 2020; 6(6):125-40. [DOI:10.29252/shenakht.6.6.125]
- Kodsi A, Bullock B, Kennedy GA, Tirlea L. Psychological interventions to improve sleep in young adults: A systematic review and meta-analysis of randomized controlled trials. Behavioral Sleep Medicine. 2022; 20(1):125-42. [PMID]
- Saruhanjan K, Zarski AC, Bauer T, Baumeister H, Cuijpers P, Spiegelhalder K, et al. Psychological interventions to improve sleep in college students: A meta-analysis of randomized controlled trials. Journal of Sleep Research. 2021, 30(1):e13097. [DOI:10.1111/jsr.13097] [PMID]
- Murawski B, Wade L, Plotnikoff RC, Lubans DR, Duncan MJ. A systematic review and meta-analysis of cognitive and behavioral interventions to improve sleep health in adults without sleep disorders. Sleep Medicine Reviews. 2018; 40:160-9. [DOI:10.1016/j.smrv.2017.12.003] [PMID]
- Hansen K, Höfling V, Kröner-Borowik T, Stangier U, Steil R. Efficacy of psychological interventions aiming to reduce chronic nightmares: A meta-analysis. Clinical Psychology Review. 2013; 33(1):146-55. [DOI:10.1016/j.cpr.2012.10.012] [PMID]
- Farrokhi H, Mostafapour V, Bondar Kakhki Z. [The effectiveness of multi-component cognitive-behavior therapy for insomnia on the elderly people suffering from insomnia (Persian)]. Journal of School of Public Health and Institute of Public Health Research. 2018; 16(2):138-47. [Link]
- Carney CE, Edinger JD, Krystal AD, Stepanski EJ, Kirby A. The contribution of general anxiety to sleep quality ratings in insomnia subtypes. Sleep. 2006; 29(1):233-42. [Link]
- Edinger JD, Fins AI, Glenn DM, Sullivan RJ Jr, Bastian LA, Marsh GR, et al. Insomnia and eye of beholder: Are there clinical markers of objective sleep disturbances among adults with and without insomnia complaints? Journal of Consulting and Clinical Psychology. 2000; 68(4):586-93. [PMID]
- Gleason K, McCall WV. Current concepts in the diagnosis and treatment of sleep disorders in the elderly. Current Psychiatry Reports. 2015, 17(6):45. [DOI:10.1007/s11920-015-0583-z] [PMID]
- Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. Journal of Clinical Sleep Medicine. 2008, 4(5):487-504 [DOI:10.5664/jcsm.27286] [PMID] [PMCID]
- Golafrooz M, Sadeghi H, Mousavi SQ, Tabaraee Y. [The effect of using continuous care model on sleep quality in people with type 2 diabetes (Persian)]. Journal Of Sabzevar University Of Medical Sciences. 2014; 21(4):655-64. [Link]
- Mottaghi R, Kamkar A, Maredpoor A. [Effectiveness of targeted musical therapy on sleep quality and overcoming insomnia in seniors (Persian)]. Salmand: Iranian Journal of Ageing. 2016; 11(2):348-57. [DOI:10.21859/sija-1102348]
- Nilsson U. Soothing music can increase oxytocin levels during bed rest after open-heart surgery: A randomised control trial. Journal of Clinical Nursing. 2009; 18(15):2153-61. [DOI:10.1111/j.1365-2702.2008.02718.x] [PMID]
- Wang CF, Sun YL, Zang HX. Music therapy improves sleep quality in acute and chronic sleep disorders: A meta-analysis of 10 randomized studies. International Journal of Nursing Studies. 2014; 51(1):51-62. [DOI:10.1016/j.ijnurstu.2013.03.008] [PMID]
- Roozbahani T, Norian M, Saatchi K, Moslemi A. [Effects of progressive muscle relaxation on sleep quality in pre-university students: A randomized clinical trial (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2016; 24(1) :16-23 [DOI:10.20286/nmj-24013]
- Shafiee Z, Babaee S, Nazari A, Atashi V. [The effect of massage therapy on sleep quality of patients after coronary artery bypass graft operation (Persian)]. Iranian Journal of Cardiovascular Nursing. 2013; 2(2):22-9. [Link]
- Tsay SL, Rong JR, Lin PF. Acupoint massage in improving the quality of sleep and quality of life with end stage renal disease. Journal of Advance Nursing. 2003; 42(2):134-42. [DOI:10.1046/j.1365-2648.2003.02596.x] [PMID]
- Tsay SL, Chen Ml. Acupressure and quality of sleep in patient in with end stage renal disease: A randomized controlled trial. International Journal of Nursing Studies. 2003; 40(1):1-7. [DOI:10.1016/S0020-7489(02)00019-6]
- Motavakel N, Maghsoudi Z, Mohammadi Y, Oshvandi K. [The effect of spiritual care on sleep quality in patients with multiple sclerosis referred to the MS Society of Hamadan city in 2018 (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2020; 28(1):36-45. [DOI:10.30699/ajnmc.28.1.36]
- Tartibian B, Heidary D, Mehdipour A, Akbarizadeh S. [The effect of exercise and physical activity on sleep quality and quality of life in Iranian Older Adults: A systematic review (Persian)]. Journal of Gerontology. 2021; 6(1):18-31. [Link]
- Bahraini S, Naji SA, Mannani R, Bekhradi R. [The effect of massage therapy on the quality of sleep in women with multiple sclerosis being admitted by Isfahan M.S. Association (Persian)]. Journal Of Urmia Nursing and Midwifery Faculty. 2011; 8(4):197-203. [Link]
- Saeedi M, Ashktorab T, Saatchi K, Zayeri F, Akbari S AA. [The effect of progressive muscle relaxation on sleep quality of patients undergoing hemodialysis (Persian)]. Iranian Journal of Critical Care Nursing. 2012; 5(1):23-8. [Link]
- Shafaat N, Makvand Hosseini S, Rezaei AM. [Effectiveness of multi-components cognitive-behavioral therapy on insomnia intensity and quality of sleep among breast cancer patients after surgery (Persian)]. Journal of Research in Psychological Health. 2017; 11(2):82-91. [DOI:10.29252/rph.11.2.82]
- Mahdavi M, Bagholi H. [Comparing the effectiveness of cognitive behavioral group therapy and mindfulness therapy on sleep quality of multiple sclerosis patients (Persian)]. Journal of Clinical Psychology. 2020; 11(4):67-76. [DOI:10.22075/JCP.2019.18600.1723]
- Babahaji M, Tayebi A, Ebadi A, Askari S, Ebrahimi S, Sharafi S. [Effect of Hathayoga exercise on sleep quality of hemodialysis patients (Persian)]. Iranian Journal of Nursing Research. 2014; 9(3):1-9. [Link]
- Hasani Sadi S, Vaezi A. [Study of the effect of yoga exercises on anxiety and sleep quality of patients with chronic heart failure in Kerman city in 2015 (Persian)]. Daneshvar Medicine. 2017; 24(126):35-45. [Link]
- Jalal Manesh S, Zargarani F. [Effectsofprogressivemusclerelaxationtechniqueonfatigueandsleepquality in patientswithmultiplesclerosis (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2015; 23(3):5-14. [Link]
- Afshar M, Mmohsenzade A, Srafraz N. [The effect of guided imagery on anxiety and sleep quality in hemodialysis patients: A randomized clinical trial (Persian)]. Qom University of Medical Sciences Journal. 2020; 13(11):59-67. [Link]
- Khodadoost M, Negaresh R, Mokhtarzade M, Ranjbar R. [Investigation moderator effect of body composition and gender on improvement of sleep quality, sleepiness and quality of life during aerobic interval training program in people with multiple sclerosis (Persian)]. Jundishapur Scientific Medical Journal. 2019; 18(5):491-506. [DOI: 10.22118/JSMJ.2019.203700.1851]
- Moradi Mohammadi F, Bagheri H, Khosravi A, Ameri M, Khajeh MM. [The effect of benson relaxation technique on sleep quality after coronary artery bypass graft surgery (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2020; 27(6):371-80. [DOI:10.30699/ajnmc.27.6.371]
- Mehdizadeh S, Salaree M, Ebadi A, Aslani J, Naderi Z, Jafari Varjoshani N. [Effect of using continuous care model on sleep quality of chemical warfare victims with bronchiolitis obliterans (Persian)]. Journal of Hayat. 2010; 16(2):5-14.[Link]
- Borzou S, Khavari F, Tapak L. [The effects of sleep hygiene education on fatigue and sleep quality in hemodialysis patients: A quasi experimental study (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2019; 27(1):25-34. [DOI:10.30699/ajnmc.27.1.25]
- Ariamanesh F, Malekshahi F, Safari M. [The effect of foot massage on night sleep quality in hemodialysis patients (Persian)]. Yafte. 2015; 17(1):71-7. [Link]
- Akbarzadeh R, Koushan M, Rakhshani MH, Hashemi Nik SM. [Effect of the benson relaxation technique on quality of sleep in patients with chronic heart disease (Persian)]. Journal of Sabzevar University of Medical Sciences. 2014; 21(3):492-50. [Link]
- Ranjbaran S, Dehdari T, Sadeghniiat Haghighi KH, Mahmoudi Majdabadi M. [Effect of cardiac rehabilitation program on quality of sleep in patients with coronary artery bypass graft surgery (Persian)]. Preventive Care in Nursing & Midwifery Journal. 2015; 5(1):37-45.[Link]
- Kashi MS, Sedghi Goyaghaj N, Hoseini MA, Mohammadi Shahbolaghi F, Bakhshi E. [Effect of jaw relaxation on sleep quality in patients with myocardial infarction(Persian)]. Medical - Surgical Nursing JournaL. 2016; 4(4):57-64. [Link]
- Radman E, Khodabakhshi Koolaee A, Taghvaee D. [Effectiveness of the anger management group therapy on sleep quality and anger among the patients with coronary heart diseases (Persian)]. Commonity HealtH. 2015; 2(4):228-37. [Link]
- Hadadian F, Jalalvandi F, Ghobadi A, Taimazy F, Panahifar S. [Effect of progressive muscle relaxation technique on sleep quality in hemodialysis patients in Kermanshah, 2011 (Persian)]. Journal of Clinical Research in Paramedical Sciences. 2015; 4(2):120-7. [Link]
- Pahlavan AR, Ahi Q. [Effectiveness of positive psychology interventions on death anxiety and sleep quality of female patients with multiple sclerosis (Ms) (Persian)]. Research In Clinical Psychology and Counseling (Studies In Education & Psychology ). 2020; 9(2 ):28-42. [Link]
- Zargarani F, Kamkar M, Maghsoudlou A. [The effect of progressive muscle relaxation technique on the quality of sleep and fatigue in patients with multiple sclerosis (Persian)]. Nursing and Midwifery Journal. 2018; 15(12):911-20. [Link]
- Baghaei R, Moradi Y, Majidi VS. [The effect of sleep hygiene education on sleep quality of patients with heart failure hospitalized in cardiac care units of Urmia teaching hospitals 2017-2018 (Persian)]. Nursing and Midwifery Journal. 2019; 17(9):674-89. [Link]
- Sanagouye Moharer G, Kia S, Akbarizadeh A, Erfani M. [Effect of hope therapy on sleep quality, subjective well-being and health hardiness among cancer patients with breast evacuation (Persian)]. Iranian Journal of Rehabilitation Research in Nursing. 2019; 6(2):66-73. [Link]
- Ghiasvandian S, Haghverdi R, Zakerimoghadam M, Kazemnezhad A, Mousavi M, Saeid Y. [The effect of preferred music on sleep quality among patients after coronary artery bypass surgery (Persian)]. Iranian Journal of Cardiovascular Nursing . 2014; 3(3):14-21. [Link]
- Cheraghi M, Akbari K, Bahramnezhad F, Haghani H. [The effect of instrumental music on sleep in patients admitted to coronary care unit (Persian)]. Iranian Journal Of Cardiovascular Nursing. 2015; 3(4):24-33. [Link]
- Zakeri moghadam M, Mousavi malek N, Esmaeeli M, Kazem Nejad A. [The effect of supportive educational intervention on sleep before coronary artery bypass graft surgery (Persian)]. Iranian Journal of Cardiovascular Nursing. 2016; 4(4):40-7. [Link]
- Saeedi Taheri Z, Asadzandi M, Ebadi A. [The effect of spiritual care based on Ghalbe Salim Model on the sleep quality of the patients with coronary artery disease (Persian)]. Journal of Critical Care Nursing. 2014; 7(2):92-101. [Link]
- Memarian R, Elhani F, Janat Alipour Z. [The effect of designed care plan on sleep situation of hospitalization preschool children with leukemia (Persian)]. Daneshvar Medicine. 2004; 11(48):45-52. [Link]
- Elahiyan Borojeni E, Afrasiabifar A, Najafi Doulatabad S, MousaviZadeh A. [The effect of the movie- based education on sleep quality in patients with bronchial asthma (Persian)]. Armaghan-e- Danesh. 2017; 22(2):176-88. [Link]
- Balazadeh R, Akbari B, Abolghasemi A. [Effectiveness of Stress management based on cognitive-behavioral training on sleep quality and cognitive bias of patients with primary hypertension (Persian)]. Journal of North Khorasan University of Medical Sciences. 2020; 11(4):14-20. [Link]
Type of Study: Review |
Subject:
Mental Health
Received: 2021/08/30 | Accepted: 2022/02/27 | Published: 2022/04/1
Received: 2021/08/30 | Accepted: 2022/02/27 | Published: 2022/04/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





