

Volume 28, Issue 4 (Autumn 2022)
Intern Med Today 2022, 28(4): 434-447 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadzadeh A, Sharifi Mood F, Tamiz Tousi D, Nemati Shahri F, Moshari J, Mardaneh J et al . Investigating Gastrointestinal Symptoms and Laboratory Findings Related to COVID-19 in Patients Referred to Allameh Bahloul Gonabadi Hospital, Iran. Intern Med Today 2022; 28 (4) :434-447
URL: http://imtj.gmu.ac.ir/article-1-3856-en.html
URL: http://imtj.gmu.ac.ir/article-1-3856-en.html
Alireza Mohammadzadeh1 

 , Farnoosh Sharifi Mood2
, Farnoosh Sharifi Mood2 

 , Delara Tamiz Tousi3
, Delara Tamiz Tousi3 

 , Fatemeh Nemati Shahri4
, Fatemeh Nemati Shahri4 

 , Jalil Moshari5
, Jalil Moshari5 

 , Jalal Mardaneh *6
, Jalal Mardaneh *6 

 , Sina Nasrollahian7
, Sina Nasrollahian7 




 , Farnoosh Sharifi Mood2
, Farnoosh Sharifi Mood2 

 , Delara Tamiz Tousi3
, Delara Tamiz Tousi3 

 , Fatemeh Nemati Shahri4
, Fatemeh Nemati Shahri4 

 , Jalil Moshari5
, Jalil Moshari5 

 , Jalal Mardaneh *6
, Jalal Mardaneh *6 

 , Sina Nasrollahian7
, Sina Nasrollahian7 


1- Department of Microbiology, Infectious Diseases Research Center, School of Medicine, Gonabad University of Medical Sciences, Gonabad, Iran.
2- Infectious Diseases Research Center, Gonabad University of Medical Sciences, Gonabad, Iran.
3- Student Research Committee, School of Medicine, Gonabad University of Medical Sciences, Gonabad, Iran.
4- Central Laboratory Research, Gonabad University of Medical Sciences, Gonabad, Iran.
5- Department of Pediatrics, School of Medicine, Gonabad University of Medical Sciences, Gonabad, Iran.
6- Department of Microbiology, Infectious Diseases Research Center, School of Medicine, Gonabad University of Medical Sciences, Gonabad, Iran. ,jalalmardaneh@yahoo.com
7- Department of Bacteriology and Virology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
2- Infectious Diseases Research Center, Gonabad University of Medical Sciences, Gonabad, Iran.
3- Student Research Committee, School of Medicine, Gonabad University of Medical Sciences, Gonabad, Iran.
4- Central Laboratory Research, Gonabad University of Medical Sciences, Gonabad, Iran.
5- Department of Pediatrics, School of Medicine, Gonabad University of Medical Sciences, Gonabad, Iran.
6- Department of Microbiology, Infectious Diseases Research Center, School of Medicine, Gonabad University of Medical Sciences, Gonabad, Iran. ,
7- Department of Bacteriology and Virology, School of Medicine, Shiraz University of Medical Sciences, Shiraz, Iran.
Full-Text [PDF 3853 kb]
(684 Downloads)
| Abstract (HTML) (1611 Views)
Full-Text: (543 Views)
Introduction
In December 2019, a novel coronavirus known as SARS-CoV-2 was spread as a highly contagious pneumonia across China and quickly throughout the world [1]. Since 2020, Iran has been one of the first countries to be infected with the virus [2]. Most of the SARS-CoV-2 infected patients develop a mild to moderate illness and the majority of cases recover without hospitalization [3]. The clinical spectrum and symptoms of COVID-19 are wide. Common symptoms are fever, dry cough, and fatigue, while less common symptoms include pain, sore throat, diarrhea, conjunctivitis, headache, loss of sense of smell and taste, rash on the skin, or discoloration of the fingers and toes [4]. Although SARS-CoV-2 infection is mainly a respiratory infection and pulmonary manifestations are the main presentation, this infection is not limited to the respiratory system and other organs can be affected. Recent studies of COVID-19 showed that digestive symptoms are present in a significant number of patients and recent observations with COVID-19 indicated that some patients present digestive symptoms as the only presentation of the illness without respiratory symptoms. Angiotensin converting enzyme 2 (ACE2) has an important role in cellular infection with the SARS-CoV-2 virus [5]. Several studies have revealed that the virus enters the host target cells via ACE2. ACE2 is expressed to be widely available across tissues, but it is specific to the intestine where it is enriched at nearly 100-fold higher levels compared to respiratory organs [1]. SARS-CoV-2 can disrupt ACE2 activity and cause intestinal epithelium infection by inducing cytotoxicity. Then, the virus can cause digestive symptoms and viral shedding in stools [6]. Due to the importance of COVID-19 infection in terms of its extensive spread, as a significant pandemic, and high mortality rate especially among high-risk patients, this descriptive, cross-sectional study aims to investigate gastrointestinal symptoms, laboratory findings, and imaging associated with COVID-19 on patients referred to Allameh Bahloul Gonabadi Hospital in 2019-2021.
Materials and Methods
Patients and study design
This descriptive, cross-sectional single-center study was conducted in Gonabad City, Iran. A total of 45 454 medical records of hospitalized COVID-19 patients in Bohlool Hospital from 2019 to 2021 were examined. Of those, 911 subjects with gastrointestinal symptoms, and finally via the simple random sampling method, 235 patients with COVID-19 and gastrointestinal symptoms were selected and included in the present study. Patients with a confirmative real-time polymerase chain reaction result for SARS-CoV-2 infection were accepted for the study and patients with incomplete information were excluded.
Data collection
The data were extracted by using a demographic questionnaire and checklist for laboratory results from the hospital-referred patients. The following information was collected: demographic information (age and sex) along with clinical, laboratory, and radiological findings. The clinical data included primary clinical as well as gastrointestinal symptoms. Laboratory information included complete blood count and routine blood biochemistry information, such as white blood cell (WBC), platelets (Plt), erythrocyte sedimentation rate (ESR), prothrombin time (PT), partial thromboplastin time (PTT), international normalized ratio (INR), alanine transaminase (ALT), aspartate aminotransferase (AST), lactate dehydrogenase (LDH), C-reactive protein (CRP), and serum ferritin. Radiological findings included diagnostic results of chest computed tomography (CT) scans. Only the first laboratory findings and CT scan results after hospitalization were used in the present study.
Statistical analysis
Statistical analyses were performed using the SPSS software, version 20 (SPSS Inc., Chicago, Ill., USA). Quantitative variables were presented as central indicators Mean±SD and to describe qualitative variables, the data were expressed as frequency (counts %).
Results
Demographic and epidemiological characteristics
A total of 235 hospitalized patients with positive real-time polymerase chain reaction result at Allameh Bahloul Gonabadi Hospital (Gonabad, Iran) from 2019 to 2021 were included in this study. The age of the cases was in the range of 1 to 97 years, with a Mean±SD age of 59.62±12.20 years (Table 1).
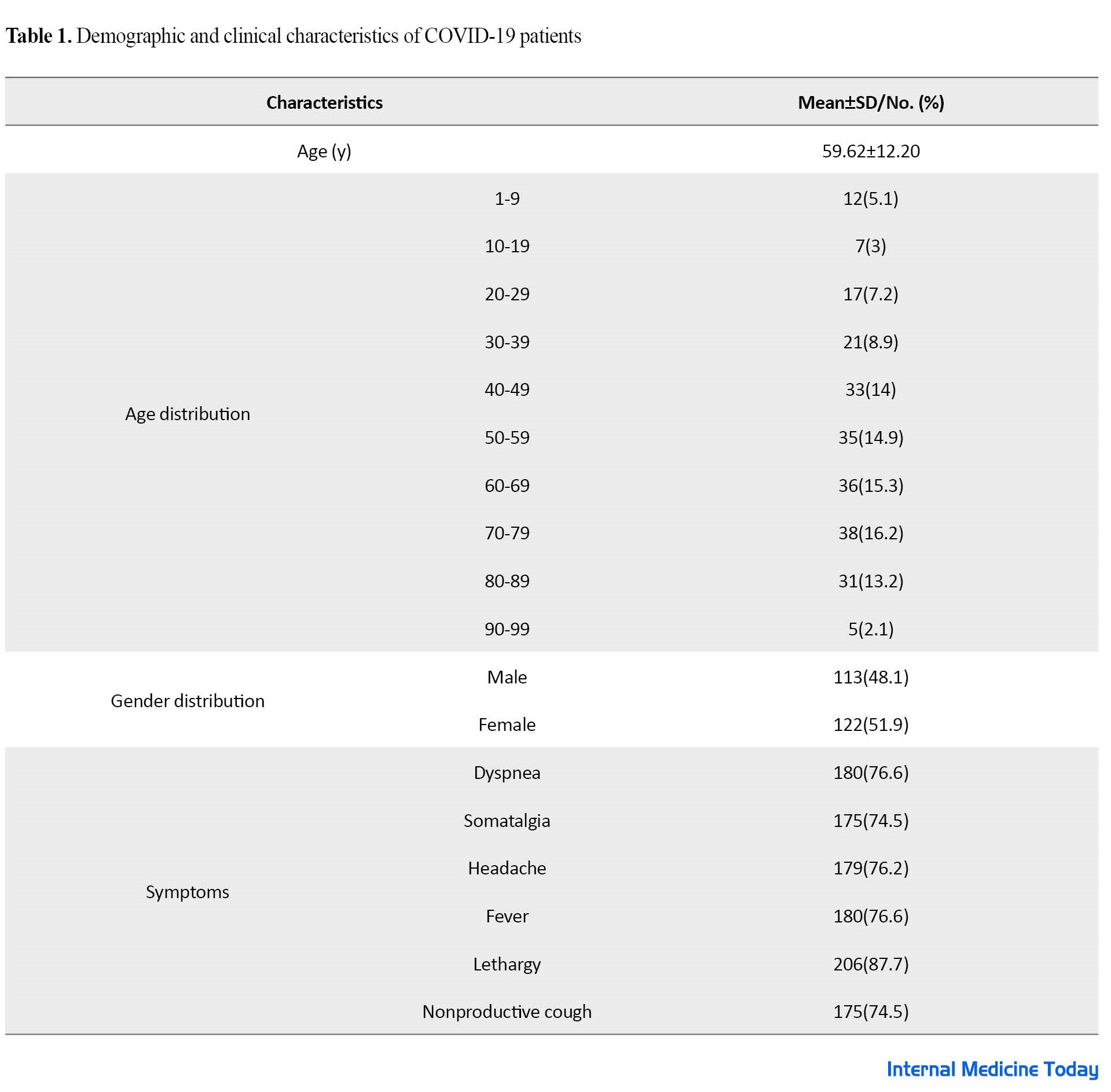
The oldest age group (16.2%) was 70-79 years old, and the gender split was 113(48.1%) men and 122(51.9%) women. The clinical features are summarized in Table 1. The most common symptoms were lethargy (87.7%), dyspnea (76.6%), and fever (76.6%).
Gastrointestinal signs and symptoms
Acceptable gastrointestinal symptoms were defined as nausea, vomiting, anorexia, abdominal pain, and diarrhea. A total of 20.04% of patients had gastrointestinal symptoms. Nausea was the most common gastrointestinal symptom which was reported in 45.1% of the patients, followed by vomiting (16.6%). Only 9.8% of the patients had diarrhea (Table 2).

Laboratory findings
According to Table 3, the increased LDH (96.6), CRP and ECR (83.8), AST (75.7), PT (46.8), and INR (42.8), followed by decreased WBC (25.7%), PLt (23%), and lymphocytes (68.5%) were the most important laboratory findings of COVID-19 patients (Table 3).

CRP results were negative in 60 patients (25.5%), one plus (1+) positive in 63 patients (26.8%), two plus (2+) positive in 70 patients (29.8%), and three plus (3+) positive in 42 patients (17.9%), according to serology (Figure 1).
Chest CT scan
Of 235 study participants, 170 patients had a chest CT scan and of these, 9 patients (3.5%) with no lung involvement and 161 patients (94.7%) had varying degrees of lung involvement.
Discussion
Given the importance of clinical symptoms, laboratory findings, and imaging data as critical knowledge that should be studied when a new infectious disease emerges [7], we conducted this study on hospitalized COVID-19 patients at Allameh Bahloul Gonabadi Hospital (Gonabad, Iran) from 2019 to 2021. In the present study, 51.9% of the patients were female and no statistically significant difference was observed between the frequency of male and female which was a contrast to the results of previous studies. Previous research showed that male subjects are more susceptible to the disease than females [8-11]. Several studies showed that different gastrointestinal symptoms were part of the clinical manifestation of SARS-CoV-2 infection [11-14]. In the present study, the prevalence of gastrointestinal symptoms among COVID-19 patients was 20.04%, and the most common gastrointestinal symptom in these subjects was nausea (31.6%) followed by vomiting (17.8%) and anorexia (9.9%). This is while some studies have reported diarrhea as the most common manifestation [11]. The most important laboratory findings observed in our study were elevated levels of CRP, ESR, and LDH in COVID-19 patients. In the present study, ECR and CRP were increased in 83.8% of patients. A meta-analysis involving 21 studies conducted by Henry et al. showed that ESR and CRP were significantly elevated in patients with severe COVID-19 [15]. The study by Fei et al. in 2020 indicated that COVID‐19 patients were associated with high levels of ESR, CRP, and LDH [16]. CRP plays a positive role in the inflammatory response and helped the human body to have non-specific resistance to overcome the virus. As a result, infectious diseases are on the rise. Consistent with our findings, recent studies show that SARS-CoV-2 infection caused a significant increase in CRP and CRP that leads to an increase in ESR. CRP as an acute inflammatory factor, has a crucial role in the diagnosis and treatment of infectious diseases and ESR is the most powerful factor that has heretofore been identified to predict COVID-19 infection progression of patients. In this study, LDH is the most frequently elevated (96.6%). According to the Zhang study in 2020 on the laboratory findings of COVID-19, the levels of LDH in 46.2% of patients with COVID-19 increased. Therefore, it can be concluded that the level of LDH in the patients is an independent risk factor for SARS-CoV-2 [17]. Leukocytosis and leukopenia are often observed in patients with COVID-19. In the study of Yamada et al., it was reported that leukocytosis was associated with severe COVID-19 infection and it could be a biomarker to predict severe COVID-19. Meanwhile, leukopenia is associated with a good prognosis of COVID-19 infection [18]. In the present study, in terms of WBC variation in COVID-19 patients, 25.7% had decreased WBC (leukopenia) and 15.3% had increased WBC (leukocytosis). WBC variation in COVID-19 patients could be different because of the severity of the illness (hospitalization or outpatient) and the presence or absence of clinical manifestations that may explain the fluctuations reported in our study and other studies. In our study, 68.5% of patients showed a decreased count of lymphocytes which is consistent with the results of Wang et al. (72% of COVID-19 patients with lymphocytopenia) [19]. A meta-analysis study of Huang et al. showed that the counts of lymphocyte subsets are significantly decreased in severe COVID-19 illness and lymphocytopenia is a dependable indicator of primary SARS CoV-2 infection [20]. Fan et al. reported abnormal liver tests (increased levels of ALT, AST, GGT, ALP, and TBILI) in COVID-19 patients for the first time [21]. In our study, the rate of increased AST and ALT in COVID-19 patients was 45.7% and 47.7%, respectively. Thrombocytopenia was observed in 23% of the patients in our study. According to the study by Karimi Shahri et al., thrombocytopenia is commonly found in 5% to 40% of patients with COVID-19 [22]. A chest CT scan is useful in determining the diagnosis and prognosis of COVID-19 [23]. Of 235 study participants, 170 patients had a chest CT scan and of these, 9 patients (3.5%) with no lung involvement and 161 patients (94.7%) had varying degrees of lung involvement. Lung involvement is the most obvious symptom, which can be seen with a CT scan. A total of 75 patients in the current study did not have a lung CT scan which demonstrates a limitation of our study. This study examined clinical symptoms and laboratory findings data of COVID-19 in hospitalized patients, which has value for planning to provide health care and preventive interventions along with subjects for future research.
Conclusion
The COVID-19 infection may present with various gastrointestinal manifestations in patients. This descriptive, cross-sectional study showed that gastrointestinal symptoms, including nausea, vomiting, and anorexia, are common complaints in patients with COVID-19, and the most common laboratory findings in patients with COVID-19 were increased LDH, CRP, ESR, and AST and decreased WBC, PLT, and lymphocytes. Lung involvement is the most obvious, which can be observed with a CT scan.
Ethical Considerations
Compliance with ethical guidelines
This paper was approved by the Ethics Committee of Gonabad University of Medical Sciences (Code: IR.GMU.REC.1400.052). In this study, confidentiality of patient information was respected.
Funding
This study was financially supported by the Gonabad University of Medical Sciences (Grant No.: 93.116.P.A).
Authors' contributions
All authors equally contributed to this project.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors appreciate the sincere cooperation of colleagues in the laboratory of Allameh Bahloul Gonabadi Hospital.
References
In December 2019, a novel coronavirus known as SARS-CoV-2 was spread as a highly contagious pneumonia across China and quickly throughout the world [1]. Since 2020, Iran has been one of the first countries to be infected with the virus [2]. Most of the SARS-CoV-2 infected patients develop a mild to moderate illness and the majority of cases recover without hospitalization [3]. The clinical spectrum and symptoms of COVID-19 are wide. Common symptoms are fever, dry cough, and fatigue, while less common symptoms include pain, sore throat, diarrhea, conjunctivitis, headache, loss of sense of smell and taste, rash on the skin, or discoloration of the fingers and toes [4]. Although SARS-CoV-2 infection is mainly a respiratory infection and pulmonary manifestations are the main presentation, this infection is not limited to the respiratory system and other organs can be affected. Recent studies of COVID-19 showed that digestive symptoms are present in a significant number of patients and recent observations with COVID-19 indicated that some patients present digestive symptoms as the only presentation of the illness without respiratory symptoms. Angiotensin converting enzyme 2 (ACE2) has an important role in cellular infection with the SARS-CoV-2 virus [5]. Several studies have revealed that the virus enters the host target cells via ACE2. ACE2 is expressed to be widely available across tissues, but it is specific to the intestine where it is enriched at nearly 100-fold higher levels compared to respiratory organs [1]. SARS-CoV-2 can disrupt ACE2 activity and cause intestinal epithelium infection by inducing cytotoxicity. Then, the virus can cause digestive symptoms and viral shedding in stools [6]. Due to the importance of COVID-19 infection in terms of its extensive spread, as a significant pandemic, and high mortality rate especially among high-risk patients, this descriptive, cross-sectional study aims to investigate gastrointestinal symptoms, laboratory findings, and imaging associated with COVID-19 on patients referred to Allameh Bahloul Gonabadi Hospital in 2019-2021.
Materials and Methods
Patients and study design
This descriptive, cross-sectional single-center study was conducted in Gonabad City, Iran. A total of 45 454 medical records of hospitalized COVID-19 patients in Bohlool Hospital from 2019 to 2021 were examined. Of those, 911 subjects with gastrointestinal symptoms, and finally via the simple random sampling method, 235 patients with COVID-19 and gastrointestinal symptoms were selected and included in the present study. Patients with a confirmative real-time polymerase chain reaction result for SARS-CoV-2 infection were accepted for the study and patients with incomplete information were excluded.
Data collection
The data were extracted by using a demographic questionnaire and checklist for laboratory results from the hospital-referred patients. The following information was collected: demographic information (age and sex) along with clinical, laboratory, and radiological findings. The clinical data included primary clinical as well as gastrointestinal symptoms. Laboratory information included complete blood count and routine blood biochemistry information, such as white blood cell (WBC), platelets (Plt), erythrocyte sedimentation rate (ESR), prothrombin time (PT), partial thromboplastin time (PTT), international normalized ratio (INR), alanine transaminase (ALT), aspartate aminotransferase (AST), lactate dehydrogenase (LDH), C-reactive protein (CRP), and serum ferritin. Radiological findings included diagnostic results of chest computed tomography (CT) scans. Only the first laboratory findings and CT scan results after hospitalization were used in the present study.
Statistical analysis
Statistical analyses were performed using the SPSS software, version 20 (SPSS Inc., Chicago, Ill., USA). Quantitative variables were presented as central indicators Mean±SD and to describe qualitative variables, the data were expressed as frequency (counts %).
Results
Demographic and epidemiological characteristics
A total of 235 hospitalized patients with positive real-time polymerase chain reaction result at Allameh Bahloul Gonabadi Hospital (Gonabad, Iran) from 2019 to 2021 were included in this study. The age of the cases was in the range of 1 to 97 years, with a Mean±SD age of 59.62±12.20 years (Table 1).
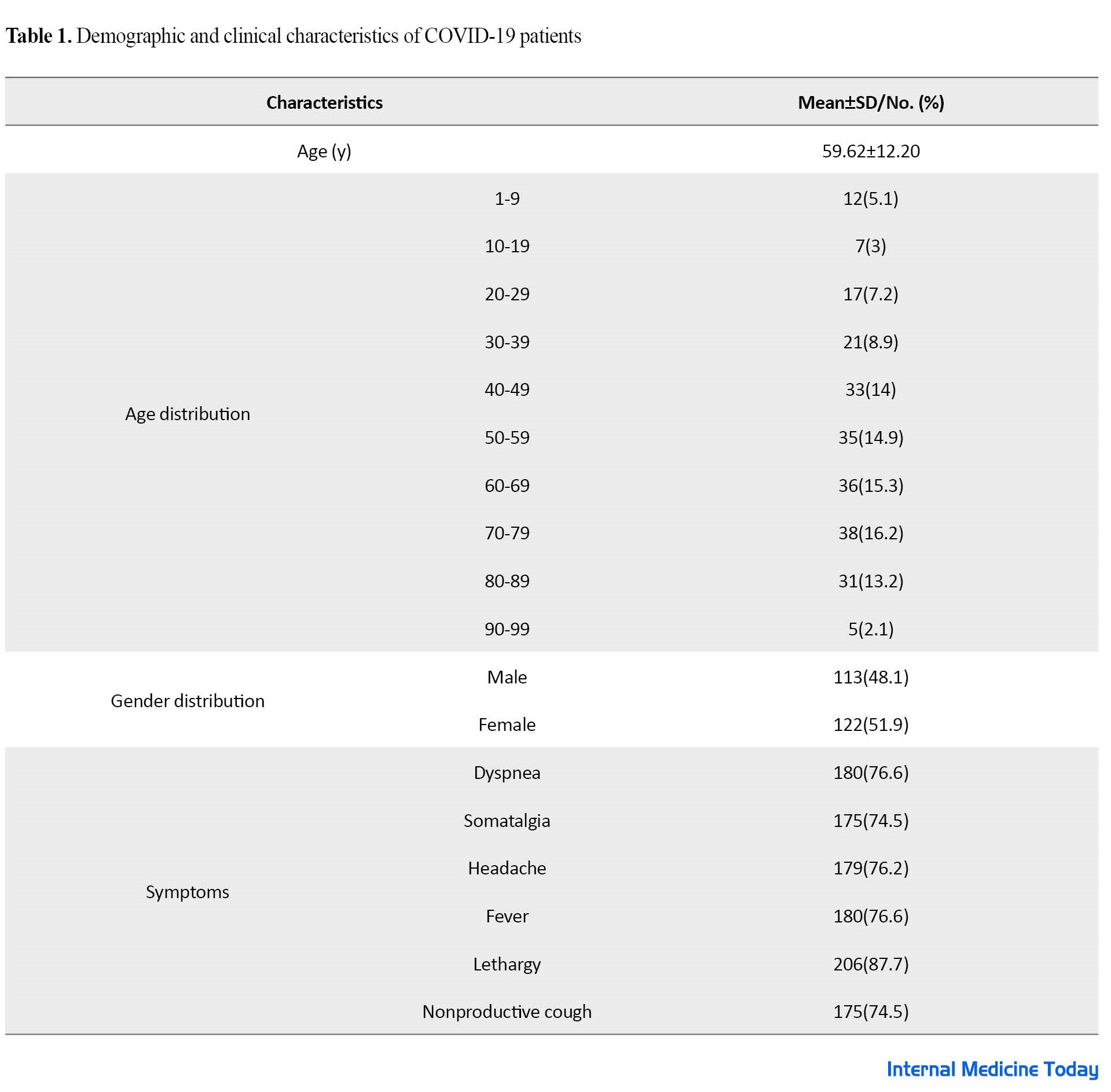
The oldest age group (16.2%) was 70-79 years old, and the gender split was 113(48.1%) men and 122(51.9%) women. The clinical features are summarized in Table 1. The most common symptoms were lethargy (87.7%), dyspnea (76.6%), and fever (76.6%).
Gastrointestinal signs and symptoms
Acceptable gastrointestinal symptoms were defined as nausea, vomiting, anorexia, abdominal pain, and diarrhea. A total of 20.04% of patients had gastrointestinal symptoms. Nausea was the most common gastrointestinal symptom which was reported in 45.1% of the patients, followed by vomiting (16.6%). Only 9.8% of the patients had diarrhea (Table 2).

Laboratory findings
According to Table 3, the increased LDH (96.6), CRP and ECR (83.8), AST (75.7), PT (46.8), and INR (42.8), followed by decreased WBC (25.7%), PLt (23%), and lymphocytes (68.5%) were the most important laboratory findings of COVID-19 patients (Table 3).

CRP results were negative in 60 patients (25.5%), one plus (1+) positive in 63 patients (26.8%), two plus (2+) positive in 70 patients (29.8%), and three plus (3+) positive in 42 patients (17.9%), according to serology (Figure 1).
Chest CT scan
Of 235 study participants, 170 patients had a chest CT scan and of these, 9 patients (3.5%) with no lung involvement and 161 patients (94.7%) had varying degrees of lung involvement.
Discussion
Given the importance of clinical symptoms, laboratory findings, and imaging data as critical knowledge that should be studied when a new infectious disease emerges [7], we conducted this study on hospitalized COVID-19 patients at Allameh Bahloul Gonabadi Hospital (Gonabad, Iran) from 2019 to 2021. In the present study, 51.9% of the patients were female and no statistically significant difference was observed between the frequency of male and female which was a contrast to the results of previous studies. Previous research showed that male subjects are more susceptible to the disease than females [8-11]. Several studies showed that different gastrointestinal symptoms were part of the clinical manifestation of SARS-CoV-2 infection [11-14]. In the present study, the prevalence of gastrointestinal symptoms among COVID-19 patients was 20.04%, and the most common gastrointestinal symptom in these subjects was nausea (31.6%) followed by vomiting (17.8%) and anorexia (9.9%). This is while some studies have reported diarrhea as the most common manifestation [11]. The most important laboratory findings observed in our study were elevated levels of CRP, ESR, and LDH in COVID-19 patients. In the present study, ECR and CRP were increased in 83.8% of patients. A meta-analysis involving 21 studies conducted by Henry et al. showed that ESR and CRP were significantly elevated in patients with severe COVID-19 [15]. The study by Fei et al. in 2020 indicated that COVID‐19 patients were associated with high levels of ESR, CRP, and LDH [16]. CRP plays a positive role in the inflammatory response and helped the human body to have non-specific resistance to overcome the virus. As a result, infectious diseases are on the rise. Consistent with our findings, recent studies show that SARS-CoV-2 infection caused a significant increase in CRP and CRP that leads to an increase in ESR. CRP as an acute inflammatory factor, has a crucial role in the diagnosis and treatment of infectious diseases and ESR is the most powerful factor that has heretofore been identified to predict COVID-19 infection progression of patients. In this study, LDH is the most frequently elevated (96.6%). According to the Zhang study in 2020 on the laboratory findings of COVID-19, the levels of LDH in 46.2% of patients with COVID-19 increased. Therefore, it can be concluded that the level of LDH in the patients is an independent risk factor for SARS-CoV-2 [17]. Leukocytosis and leukopenia are often observed in patients with COVID-19. In the study of Yamada et al., it was reported that leukocytosis was associated with severe COVID-19 infection and it could be a biomarker to predict severe COVID-19. Meanwhile, leukopenia is associated with a good prognosis of COVID-19 infection [18]. In the present study, in terms of WBC variation in COVID-19 patients, 25.7% had decreased WBC (leukopenia) and 15.3% had increased WBC (leukocytosis). WBC variation in COVID-19 patients could be different because of the severity of the illness (hospitalization or outpatient) and the presence or absence of clinical manifestations that may explain the fluctuations reported in our study and other studies. In our study, 68.5% of patients showed a decreased count of lymphocytes which is consistent with the results of Wang et al. (72% of COVID-19 patients with lymphocytopenia) [19]. A meta-analysis study of Huang et al. showed that the counts of lymphocyte subsets are significantly decreased in severe COVID-19 illness and lymphocytopenia is a dependable indicator of primary SARS CoV-2 infection [20]. Fan et al. reported abnormal liver tests (increased levels of ALT, AST, GGT, ALP, and TBILI) in COVID-19 patients for the first time [21]. In our study, the rate of increased AST and ALT in COVID-19 patients was 45.7% and 47.7%, respectively. Thrombocytopenia was observed in 23% of the patients in our study. According to the study by Karimi Shahri et al., thrombocytopenia is commonly found in 5% to 40% of patients with COVID-19 [22]. A chest CT scan is useful in determining the diagnosis and prognosis of COVID-19 [23]. Of 235 study participants, 170 patients had a chest CT scan and of these, 9 patients (3.5%) with no lung involvement and 161 patients (94.7%) had varying degrees of lung involvement. Lung involvement is the most obvious symptom, which can be seen with a CT scan. A total of 75 patients in the current study did not have a lung CT scan which demonstrates a limitation of our study. This study examined clinical symptoms and laboratory findings data of COVID-19 in hospitalized patients, which has value for planning to provide health care and preventive interventions along with subjects for future research.
Conclusion
The COVID-19 infection may present with various gastrointestinal manifestations in patients. This descriptive, cross-sectional study showed that gastrointestinal symptoms, including nausea, vomiting, and anorexia, are common complaints in patients with COVID-19, and the most common laboratory findings in patients with COVID-19 were increased LDH, CRP, ESR, and AST and decreased WBC, PLT, and lymphocytes. Lung involvement is the most obvious, which can be observed with a CT scan.
Ethical Considerations
Compliance with ethical guidelines
This paper was approved by the Ethics Committee of Gonabad University of Medical Sciences (Code: IR.GMU.REC.1400.052). In this study, confidentiality of patient information was respected.
Funding
This study was financially supported by the Gonabad University of Medical Sciences (Grant No.: 93.116.P.A).
Authors' contributions
All authors equally contributed to this project.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
The authors appreciate the sincere cooperation of colleagues in the laboratory of Allameh Bahloul Gonabadi Hospital.
References
- Zhang H, Li HB, Lyu JR, Lei XM, Li W, Wu G, et al. Specific ACE2 expression in small intestinal enterocytes may cause gastrointestinal symptoms and injury after 2019-nCoV infection. International Journal of Infectious Diseases. 2020; 96:19-24. [DOI:10.1016/j.ijid.2020.04.027] [PMID] [PMCID]
- Rassouli M, Ashrafizadeh H, Shirinabadi Farahani A, Akbari ME. COVID-19 management in Iran as one of the most affected countries in the world: Advantages and weaknesses. Frontiers in Public Health. 2020; 8:510. [DOI:10.3389/fpubh.2020.00510] [PMID] [PMCID]
- Chippa V, Aleem A, Anjum F. Post acute coronavirus (covid-19) syndrome. Treasure Island (FL): StatPearls Publishing; 2021. [PMID]
- Mehta OP, Bhandari P, Raut A, Kacimi SEO, Huy NT. Coronavirus disease (COVID-19): Comprehensive review of clinical presentation. Frontiers in Public Health. 2021; 8:582932. [DOI:10.3389/fpubh.2020.582932] [PMID] [PMCID]
- Beyerstedt S, Casaro EB, Rangel ÉB. COVID-19: Angiotensin-converting enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. European Journal of Clinical Microbiology & Infectious Diseases. 2021; 40(5):905-19. [DOI:10.1007/s10096-020-04138-6] [PMID] [PMCID]
- Ni W, Yang X, Yang D, Bao J, Li R, Xiao Y, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Critical Care. 2020; 24(1):422. [DOI:10.1186/s13054-020-03120-0] [PMID] [PMCID]
- Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Medicine and Infectious Disease. 2020; 34:101623. [DOI:10.1016/j.tmaid.2020.101623] [PMID] [PMCID]
- Haghighi M, Khoshrang H, Ghazanfar Tehran S, Aghajanzadeh P, Jafarinezhad A, Souri Z, et al. [Evaluation of epidemiological, paraclinical, and imaging findings of patients with covid-19 hospitalized in intensive care unit of Rasht Hospitals in March 2020 (Persian)]. Journal of Guilan University of Medical Sciences. 2021; 30(2):84-97. [DOI:10.32598/JGUMS.30.2.1619.2]
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. New England Journal of Medicine. 2020; 382(18):1708-20. [DOI:10.1056/NEJMoa2002032] [PMID] [PMCID]
- Li J, Huang DQ, Zou B, Yang H, Hui WZ, Rui F, et al. Epidemiology of COVID-19: A systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. Journal of Medical Virology. 2021; 93(3):1449-58. [DOI:10.1002/jmv.26424] [PMID] [PMCID]
- Pan L, Mu M, Yang P, Sun Y, Wang R, Yan J, et al. Clinical characteristics of COVID-19patients with digestive symptoms in Hubei, China: A descriptive, cross-sectional, multicenter study. The American Journal of Gastroenterology. 2020; 115(5):766-773. [DOI:10.14309/ajg.0000000000000620] [PMID] [PMCID]
- Kaafarani HM, El Moheb M, Hwabejire JO, Naar L, Christensen MA, Breen K, et al. Gastrointestinal complications in critically ill patients with COVID-19. Annals of Surgery. 2020; 272(2):e61-2. [DOI:10.1097/SLA.0000000000004004] [PMID] [PMCID]
- Aguila EJT, Cua IHY, Fontanilla JAC, Yabut VLM, Causing MFP. Gastrointestinal manifestations of COVID-19: Impact on nutrition practices. Nutrition in Clinical Practice. 2020; 35(5):800-5. [DOI:10.1002/ncp.10554] [PMID] [PMCID]
- Wang Y, Liu Y, Liu L, Wang X, Luo N, Li L. Clinical outcomes in 55 patients with severe acute respiratory syndrome coronavirus 2 who were asymptomatic at hospital admission in Shenzhen, China. The Journal of Infectious Diseases. 2020; 221(11):1770-4. [DOI:10.1093/infdis/jiaa119] [PMID] [PMCID]
- Henry BM, De Oliveira MHS, Benoit S, Plebani M, Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clinical Chemistry and Laboratory Medicine (CCLM). 2020; 58(7):1021-8. [DOI:10.1515/cclm-2020-0369] [PMID]
- Fei F, Smith JA, Cao L. Clinical laboratory characteristics in patients with suspected COVID-19: One single-institution experience. Journal of Medical Virology. 2021; 93(3):1665-71. [DOI:10.1002/jmv.26527] [PMID] [PMCID]
- Zhang ZL, Hou YL, Li DT, Li FZ. Laboratory findings of COVID-19: A systematic review and meta-analysis. Scandinavian Journal of Clinical and Laboratory Investigation. 2020; 80(6):441-7. [DOI:10.1080/00365513.2020.1768587] [PMID] [PMCID]
- Yamada T, Wakabayashi M, Yamaji T, Chopra N, Mikami T, Miyashita H, et al. Value of leukocytosis and elevated C-reactive protein in predicting severe coronavirus 2019 (COVID-19): A systematic review and meta-analysis. Clinica Chimica Acta. 2020; 509:235-43. [DOI:10.1016/j.cca.2020.06.008] [PMID] [PMCID]
- Wang F, Nie J, Wang H, Zhao Q, Xiong Y, Deng L, et al. Characteristics of peripheral lymphocyte subset alteration in COVID-19pneumonia. The Journal of Infectious Diseases. 2020; 221(11):1762-9. [PMID]
- Huang W, Berube J, McNamara M, Saksena S, Hartman M, Arshad T, et al. Lymphocyte subset counts in COVID-19 patients: A meta-analysis. Cytometry. Part A : The Journal of The International Society for Analytical Cytology. 2020; 97(8):772-6. [DOI:10.1002/cyto.a.24172] [PMID] [PMCID]
- Fan Z, Chen L, Li J, Cheng X, Yang J, Tian C, et al. Clinical features of COVID-19-related liver functional abnormality. Clinical Gastroenterology and Hepatology. 2020; 18(7):1561-6. [DOI:10.1016/j.cgh.2020.04.002] [PMID] [PMCID]
- Karimi Shahri M, Niazkar HR, Rad F. COVID-19 and hematology findings based on the current evidences: A puzzle with many missing pieces. International Journal of Laboratory Hematology. 2021; 43(2):160-8. [DOI:10.1111/ijlh.13412] [PMID] [PMCID]
- Li T, Wang X, Zhuang X, Wang H, Li A, Huang L, et al. Baseline characteristics and changes of biomarkers in disease course predict prognosis of patients with COVID-19. Internal and Emergency Medicine. 2021; 16(5):1165-72. [DOI:10.1007/s11739-020-02560-4] [PMID] [PMCID]
Type of Study: Original |
Subject:
Internal Medicine
Received: 2022/01/15 | Accepted: 2022/09/23 | Published: 2022/09/23
Received: 2022/01/15 | Accepted: 2022/09/23 | Published: 2022/09/23
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



