Volume 28, Issue 3 (Summer 2022)
Intern Med Today 2022, 28(3): 300-329 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Rahimi F, Moenimehr M. Investigating Non-Pharmacologic Treatment Methods in Reducing Anxiety in Pregnant Women of Low-Risk and High-Risk Groups: A Systematic Review. Intern Med Today 2022; 28 (3) :300-329
URL: http://imtj.gmu.ac.ir/article-1-3875-en.html
URL: http://imtj.gmu.ac.ir/article-1-3875-en.html
1- Nursing and Midwifery Sciences Development Research Center, Najafabad Branch, Islamic Azad University, Najafabad, Iran. , rahimi.farz@yahoo.com
2- Nursing and Midwifery Sciences Development Research Center, Najafabad Branch, Islamic Azad University, Najafabad, Iran.
2- Nursing and Midwifery Sciences Development Research Center, Najafabad Branch, Islamic Azad University, Najafabad, Iran.
Full-Text [PDF 8726 kb]
(1592 Downloads)
| Abstract (HTML) (2189 Views)
Full-Text: (4782 Views)
Introduction
Based on the reports provided by the World Health Organization (WHO), behavioral illnesses are the second cause of disability worldwide [1]. Mental health issues affect all societies and age groups, among which pregnant women are not an exception [2]. The mental health of the pregnant mother during pregnancy is influenced by hormonal changes and in women who consider pregnancy as a completely biological process, this is considerably joyful and gratifying. However, many women experience anxiety during this period because, during pregnancy, the individual faces major changes in their lifestyle and should create alterations in their self-image and get prepared for motherhood [3]. Based on the reported systematic reviews, mental disorders, such as depression and anxiety in women during pregnancy are more prevalent in women in low- to medium-income countries [4]. Also, the point-to-point prevalence of mental disorders during pregnancy has been reported at 14%, of which 3.3% are related to acute depression and 6.6% are related to anxiety disorders [3].
More than 50% of women experience various levels of anxiety during pregnancy, among which 8.5% to 10.5% are related to anxiety, 1.45% to 5.2% are related to fear, 1.2% to 5.1% are related to obsession and 0.3% are related to posttraumatic stress disorder [5]. Based on previous research, anxiety has been reported in 15% of Iranian pregnant women [6]. Some of the pre-existing conditions that create anxiety disorders and changes in the mental health of pregnant women are age, first-child pregnancy, physical disorders and illness, heredity, and mother-born anxiety [7], hormonal changes [8], the experience of premature childbirth and mother whose child are at great risk of abnormalities [3].
Anxiety during depression can directly affect the pattern of fetus growth and the length of pregnancy [9], or it may have significant implications, including low-weight childbirth and low Apgar score [10]. Anxiety also creates the discharge of stress hormones (adrenal steroids and corticotropin-releasing hormone) that these hormones affect the growth of the fetus’s brain growth in weeks 12 to 22 by passing the pair [11] and play a major role in premature childbirth [12]. Additionally, these hormones can cause paired vasoconstriction and limit oxygen and nutrition transfer to the fetus [11]. Meanwhile, researchers believe that stress and anxiety during pregnancy can cause vascular blood pressure and reduce the blood flow of fetus-pair while increasing the resistance of paired vessels [13]. All these factors can be the reasons for the limitation of fetus growth and fetal asphyxia [14].
In previously conducted studies, cortisol (among the stress hormones) is defined as one of the limiting factors of fetus growth [15]. High levels of anxiety in mothers and an increase in the level of cortisol hormone in amniotic fluid can affect the evolutionary process of the fetus’ brain along with social skills, communication power, and child memory in the future. Based on reports, around 15% of issues in delayed recognition and anxiety in children are the result of anxiety in the mother during pregnancy [16, 17]. The abnormal status of mental health in a pregnant woman and the existence of severe and constant anxiety cause the fetus to be exposed to glucocorticoids for a longer time and this causes constant neuroendocrine alterations in the individual. These changes can cause particular cognition or behavioral patterns and result in future problems in controlling emotions or character shocks in the fetus [18]. The study by O’Connor et al. has shown that the abnormal mental health of the mother in the 32nd week of pregnancy can cause behavioral and emotional disorders in the child up until the age of 7 years, and bring the craving symptoms in pregnant women to an uncontrollable level [19]. On the other hand, it should be noted that 20% of pregnancies can be classified as high-risk pregnancies [20]. The rate of pregnant women in the high-risk group who required special care equals 76.6% [21].
High-risk pregnant women face dangers and problems in their personal, familial, and social life and a high-risk pregnancy affects the individual and results in changes in the family functions. Evidence suggests that in high-risk pregnant women, the rate of depression is 44%, major depression 19% [22], increased rates of psychosis, anxiety, mental disorders, isolation, consumption, and sleep disorders, and fear of illness and loneliness are higher during pregnancy and after childbirth [23]. Also, in high-risk pregnant women, the possibility of the occurrence of behavioral problems is higher in their children [24]. Numerous studies have suggested nursing and obstetrics techniques as alternative treatment methods to improve mental health and reduce anxiety in pregnant women, including relaxation [9, 13-15, 25-40], mindfulness [41-55], Quran verses and spiritual treatment based on religious training [56-69], aromatherapy [70-80], consulting, spouse support and behavioral and cognition treatments [81-88] music therapy [62, 89-93], training during pregnancy and life skills [26, 35, 94-98], complementary treatments [25, 37, 38, 40, 99-106], pregnancy ball [107], KMC [108], sonography [109], supporting and accompanying pregnant mothers in the third month of school [110] and chewing gum [111, 112] .
Considering the importance of adverse effects of anxiety in pregnant women, especially high-risk pregnant women, and given the numerous studies conducted on different methods of reducing anxiety in pregnant mothers and discrepancies in the results and the lack of review studies in this field in Iran, this study aims to conduct a systematic review of conducted studies to present the best and most effective non-pharmacological methods to reduce anxiety in pregnant women at low-risk and high-risk levels in Iran and worldwide.
Materials and Methods
In this systematic review, we used all the conducted clinical trials on various types of effective non-pharmacological methods in reducing the anxiety of pregnant women in both low-risk and high-risk groups in Iran and worldwide from the beginning of 2000 to the end of 2022. The method of presenting the materials, including defining the subject, data collection, and analysis of the results, was conducted based on the PRISMA framework. To conduct the electronic search, we used time limitations. Accordingly, all published articles from the beginning of 2000 to the end of 2022 were investigated. To reach the required information from the published articles in national journals, databases of IRCT, Scopus, Irandoc, MEDLIB, Google Scholar, SID, and other articles were searched on PubMed, Science Direct, and Cochrane.
To maximize the generalizability of the search in Persian references, general and specific keywords were used as follows, anxiety, pregnancy, childbirth, mother, high-risk, clinical trial, low-risk, non-pharmacological, and their possible combinations in the abstract, title, and keywords. Accordingly, we used the operators “AND” and “OR”. For English databases the following equivalents and MeSH words were employed, “anxiety”, “pregnancy”, “delivery”, “childbirth”, “mother”, “clinical trial”, “high risk”, “low-risk”, and “non-drug”. We used the operators of “AND” and “OR” for combinatorial search. In the Google Scholar database, the keywords were entered into the subject field and all resulting articles were investigated. The inclusion criteria included being a clinical trial study and employing a method to reduce anxiety during pregnancy or childbirth in women in both groups low-risk and high-risk. To evaluate articles, we used the Jadad framework.
Results
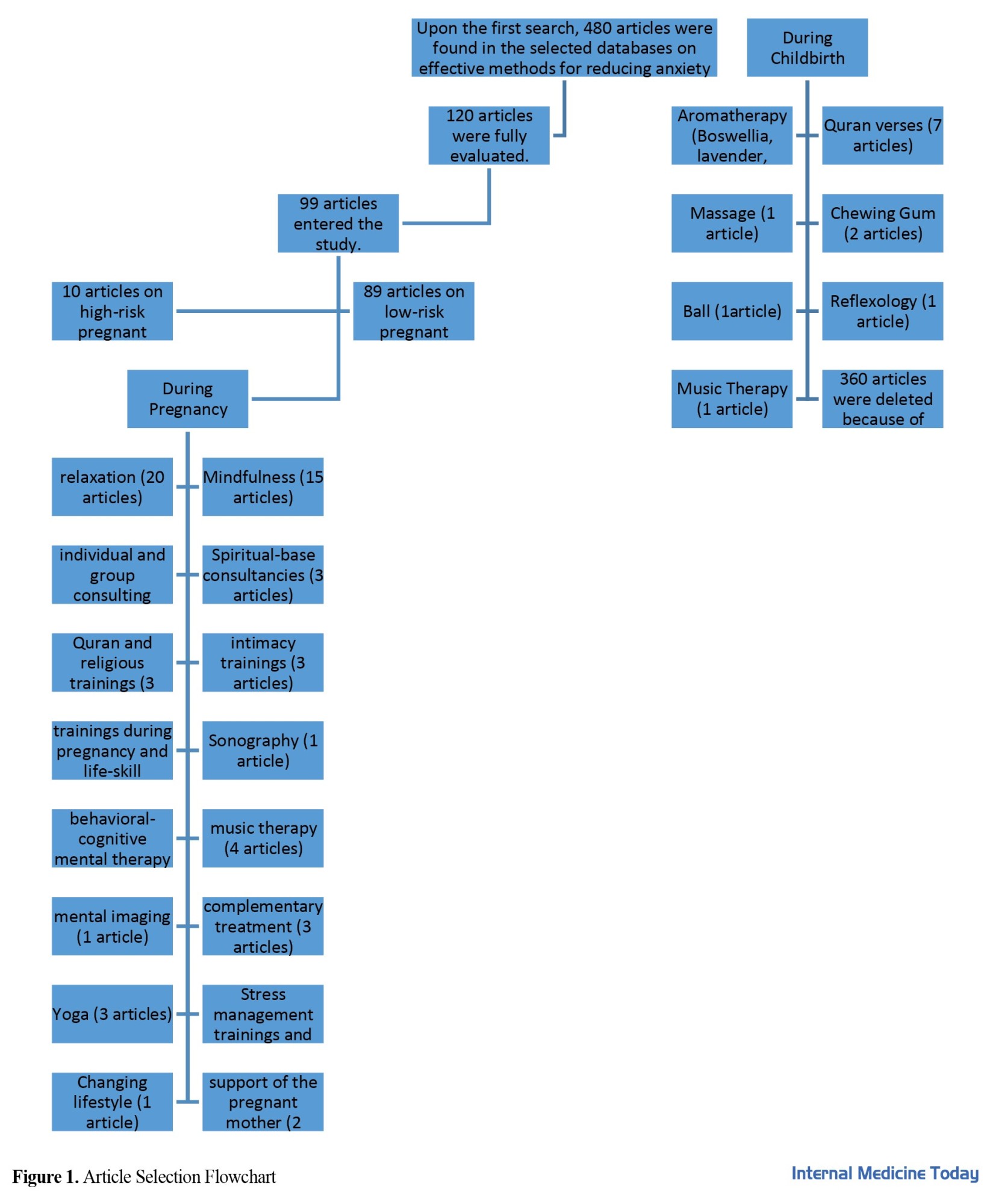
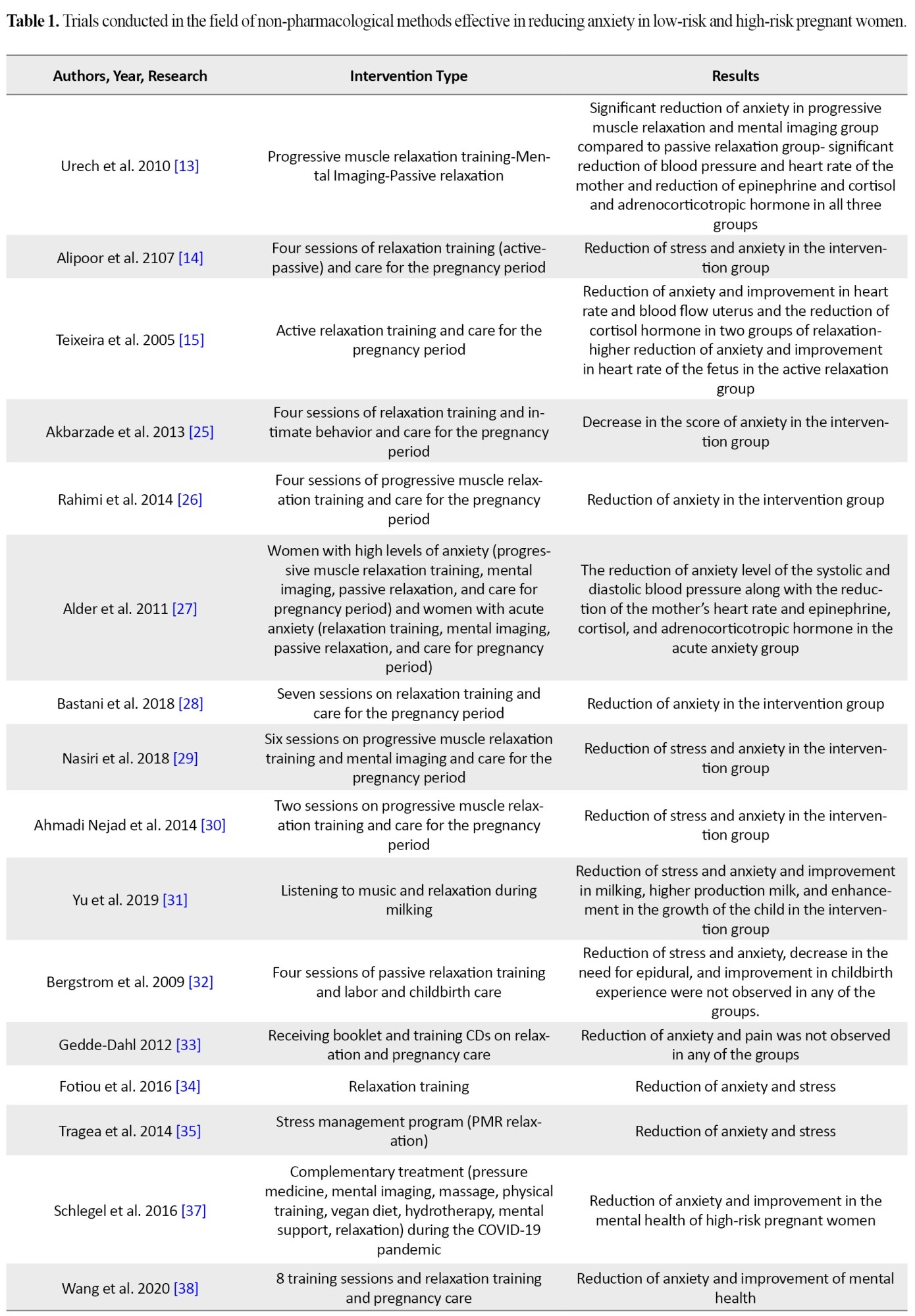
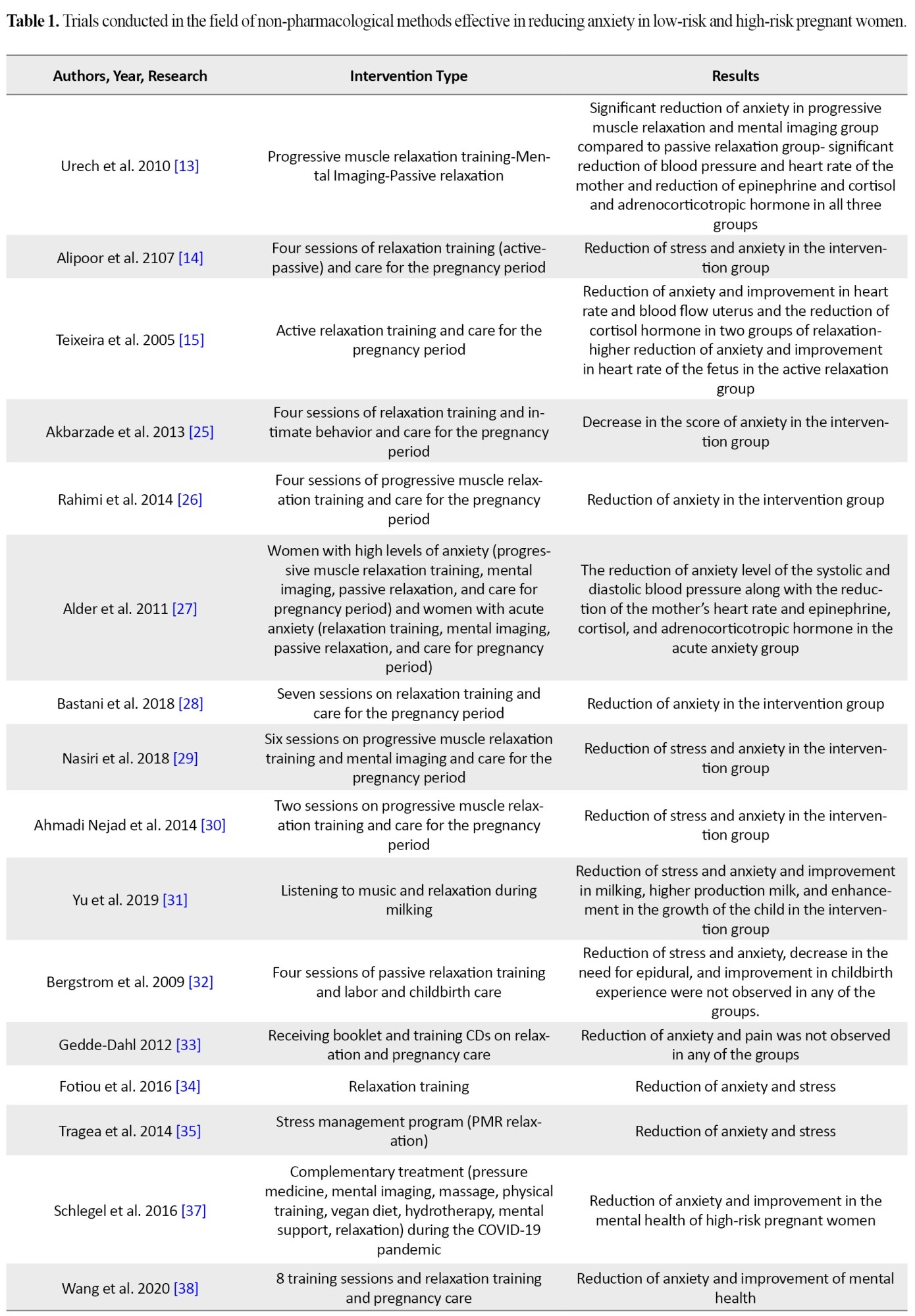
In this systematic review, a total of 120 articles were investigated. Among the investigated articles, 99 papers (52 Persian and 47 English) were selected for review. A total of 10 articles were related to high-risk pregnant women and 89 articles were conducted on low-risk pregnant women. A total of 23 different treatment methods were used to reduce anxiety in pregnant women with low-risk and high-risk during pregnancy and or the first stage of childbirth (Figure 1). In some of these studies, other variables are investigated at the same time as analyzing anxiety in pregnant women. For instance, in terms of improving the parameters of the fetus growth, 4 articles, in terms on reducing depression, 20 articles, on reducing stress, 19 articles, on improving mental health, 18 articles, on improving quality of life, 1 article, on improving sleep quality, 2 articles, and in terms of cortisol hormone level, 4 articles were conducted. Based on the investigations, the effect of relaxation (20 articles), mindfulness (15 articles), Quran verses and spiritual-based treatment based on religious training (14 articles), and aromatherapy (11 articles) along with music therapy (6 articles) were among the most frequent treatment methods in studies investigated by researchers, compared to other methods. All these methods are briefly explored in the following (Table 1).



Relaxation
Among the most common relaxation methods were progressive muscle relaxation (Jacobsen), passive relaxation, Benson relaxation, mental relaxation (Mitchel), conscious breathing, mental imaging, the method of teaching the self, and a combination of various methods. In most articles regarding the use of relaxation as an intervention, progressive muscle relaxation was employed the most. This method was designed by Edmon Jacobsen and is among the active muscle-mind relaxation methods. In muscle-mind techniques, by flexing and releasing the muscle, various parts of the body become the focus of the mind and then they are rested. In this method, the mind learns to focus on different parts of the body and remove the outside world while experiencing freeness, thereby gaining serenity. By flexing and resting the muscle, this method changes the focus of the mind from the external world to the internal world. Also, in this method, the flexing and relaxing process can be done in separation (the muscle of the tow, then the muscle of the fingers, and then the muscle of the calves, next the muscles of the thighs, etc.), in the group (multiple muscles together, for instance, the muscles of the calves and thighs, etc.), or even one half of the body (all muscles of the right side of the body and next the left side [26].
A total of 20 articles were conducted on the effect of relaxation on anxiety during pregnancy and 18 articles concluded that performing relaxation practices results in the reduction of anxiety during pregnancy [9, 13-15, 25-40] and in two articles, the reduction in anxiety during pregnancy was not reported [32, 33]. In the study by Brigstom et al. conducted in 2009 [32], performing passive relaxation did not result in stress and anxiety reduction during pregnancy, enhanced experience of pregnancy, and reduced Epidural anesthesia. In the study conducted by Gidy Dahel and Forse [33], performing relaxation did not result in reduced anxiety during pregnancy or reduced pregnancy pain and improved Apgar score. It is essential to mention that these two articles were performed on high-risk pregnant women. In the study conducted by Rahimi et al. [26], performing progressive muscle relaxations resulted in reduced anxiety in high-risk pregnant women. In the study conducted by Schiljel et al [37], performing combinatory treatments and relaxation treatments resulted in reduced anxiety in high-risk pregnant women. In addition, in the study conducted by Wang and Zahang [38], performing combinatory treatment and relaxation practice resulted in reduced anxiety and improved mental health during the COVID-19 pandemic. In the study conducted by Rafiee et al. [40], performing relaxation treatment along with intimacy training resulted in reduced anxiety in pregnant women in their third quarter.
Mindfulness
Mindfulness is an objective awareness that cannot be described and is based on the present time in terms of the experience in a particular moment in the attention span of the individual. In addition, this notion includes the confession of a remembered experience and its acceptance. In another description, mindfulness is described as a technique that along with meditation and particular mind orientations toward an experience promotes objective awareness of the present while minimizing the entanglement of thoughts and emotions [56]. Mindfulness is performed for patients to convince them that thoughts are merely thoughts and they are not reality. When they can consider their thoughts as they are and as an external phenomenon, they can view reality more clearly and manage their affairs more effectively. Mindful individuals comprehend internal and external reality more freely and without distortion and have the ability to face a wide range of thoughts, emotions, and pleasant or unpleasant experiences [53]. A total of 15 articles were conducted on the effect of mindfulness on the anxiety level in pregnant women, and all these articles concluded that mindfulness can decrease anxiety during pregnancy [41-55]. Maren Goetz et al. [51] showed that performing electronic mindfulness for a week resulted in reduced anxiety in high-risk pregnant mothers. In some of these studies, other variables, along with studying the effect of mindfulness on the anxiety of pregnant women, have been investigated, including the reduction of depression in 11 articles [41-45, 47-52], improvement in sleep quality of pregnant women in 2 studies [45, 52], the reduction of cortisol hormone in 1 article [45], the reduction of changes in the blood pressure of pregnant women in 1 article [45], the reduction of stress in pregnant women in 8 articles [41-45, 47-52], improvement in the mental health of the mothers and fathers during pregnancy in 1 article [46], enhancing self-efficacy in milking for mother in 1 article [48], and improving infant growth parameters in the article [53].
Quran verses and religious beliefs
Religious beliefs improve health, quality of life, and dependence on God. In the conducted investigations, the positive effect of religion has been reported, for instance, in women who had experienced a high-risk pregnancy. Since the religious beliefs were stronger in these individuals, hopelessness and grief were reported at lower levels [57]. In the study conducted by Niaz Azari et al. [58], group spiritual treatment in diabetic pregnant women resulted in reduced anxiety and improved quality of life. Religious beliefs and prayers positively affect the mental and physical health of the individual [57, 59]. Treatment with beliefs and faith in God for improvement is among the methods that are based on psychology and have great importance in treating illnesses and reducing pain, anxiety, and depression [57]. In the study conducted by Bodaghi et al. [59], increasing levels of spirituality in pregnant women resulted in reduced stress, anxiety, and depression in mothers. Azizi et al. [60] reported the effectiveness of religious training in the reduction of anxiety in pregnant women. Khodakarami et al. [61] indicated that spiritual-based consulting during pregnancy results in reduced stress, anxiety, and depression in mothers. Therefore, considering that pregnancy and childbirth is a sensitive period in an individual’s life, improving religious beliefs and faith can be sedative and help in the health of the mother and the baby. It is emphasized that society officials and religious leaders should participate in health promotion programs for pregnant women [57].
Quran verses
The Quran, the holy book of Muslims, considers all aspects of life, and reading it is similar to spiritual music that helps in releasing endorphins by stimulating the brain’s alpha waves. Accordingly, reading the Quran helps to eliminate negative emotions and create serenity, and strengthen the stress threshold in an individual [62]. The sound of the Quran has eloquent, simple, and elegant music that if these characteristics become available, hearers from different groups will be affected by it and their bodies and soul will be captured by it. Listening to the Quran is a systematic and complementary therapy that can help reduce stress and improve critical life symptoms [61]. In a study conducted by Naderyanfar et al. [63], listening to the Quran resulted in reduced anxiety in mothers volunteering for natural childbirth. In the review study conducted by Irani et al. [62], the sound of reading the Quran was a considerably effective factor in reducing anxiety and pain in mothers during childbirth. Employing this method has various benefits, such as less time consumption, easy access, inexpensive, noninvasive, and no danger for the patient, compared to pharmacological treatments. Abbasi et al. [64] indicated that reading the translation of Yasin Surah for 15 days results in reduced anxiety in women in their second and third quarters. Sahmeddini et al. [65] showed that listening to the sound of the Quran with headphones for 45 minutes in a maternity hospital resulted in reduced anxiety in pregnant women along with decreased serum levels of cortisol hormone. In a study conducted by Kadkhodaei et al. [66], listening to Quran sounds results in reduced anxiety in pregnant women. In the study conducted by Fitri et al. [67], listening and reading Al-Rahman Surah for 15 minutes, three times a week in the third quarter of pregnancy resulted in reduced anxiety in Indonesian pregnant women. Sohita and Mofidah [68] found that reciting Al-Rahman Surah in the active stage of pregnancy resulted in reduced anxiety and pregnancy pain in Indonesian pregnant women. In the study conducted by Mirbagher Ajorpaz and Ranjbar [69], listening to the sound of the Quran resulted in reduced anxiety in pregnant women candidates for cesarean.
Aromatherapy
Aromatherapy is a combinatory treatment method that with the help of fragrant smells and stimulating the olfactory sense results in sedation with the release of endorphins and reduces pain and anxiety [70, 71]. In addition, aromatherapy affects the hypothalamus by stimulating the olfactory sense and reduces the release of corticotropin that subsequently decreases the release of Adrenocorticotropic hormone from the hypophysis and then lowers the release of cortisol from the adrenal gland, thereby reducing anxiety [71]. In various studies, different essences have been employed. In a study conducted by Mirzae et al [72], smelling lavender resulted in reduced cortisol hormone and anxiety while increasing the level of serotonin hormone during pregnancy. In the study of Tafazoli et al., smelling lavender [73], in the study by Namazi et al., the smell of orange blossoms [70], in the study by Ozgoli et al., the smell of peppermint and clove [71], in the study of Kheirkhah et al., the smell of damask rose with hot shower [74], in the study of Sharifipour et al., the smell of common sage [75], in the study of Ozgoli et al., the smell of peppermint [76], in the study of Esmaelzadeh et al., the smell of Boswellia [77], in the study of Hamedanian et al., smelling rose [78], in the study of Rashidi Fakar et al., the smell of geraniums [79], and in the study of Rashidi Fakari et al., the smell of orange essence [80] have been reported to reduce the anxiety of pregnant mothers.
Consulting, support of the spouse, and cognitive behavioral treatments
The principles of consulting are based on listening and trying to understand the viewpoints and worries of the mother, respecting her, and trying to maintain a sympathetic and positive relationship with her [81]. In the study conducted by Moghadasi et al [81], performing support consulting resulted in reduced anxiety in mothers along with mothers who were exposed to the risk of premature childbirth. The obstetrician, as responsible, plays a crucial role in providing consultancy and care for the pregnant mother [82]. Andaroon et al. [82] showed that performing individual consulting by the obstetrician resulted in reduced anxiety in mothers during pregnancy. Consulting the pregnant mother with the spouse in terms of spiritual and mental support for the mother during pregnancy can reduce the anxiety and worries of pregnant women during pregnancy, thereby resulting in a healthier and more dynamic society with mentally and physically healthy children [83]. In the study conducted by Barjaste and Moghadam [83], performing couple consultations based on the support of the spouse resulted in reduced anxiety and worries of the pregnant mother. In the study conducted by Mohammadpour et al. [84], performing spouse consulting resulted in reduced anxiety in mothers during pregnancy.
In cognitive-behavioral treatments, individuals distance themselves from negative thoughts and try to participate in activities and obtain dominance, thereby resulting in the reduction of anxiety [85]. In the study conducted by Imanparast et al. [85], performing cognitive-behavioral treatments results in reduced anxiety in mothers. In the study conducted by Mationecsicar [86], performing positive cognitive-behavioral intervention results in reduced anxiety and stress while improving the mental health status of pregnant mothers. In the study conducted by Ghorbani et al. [87], performing group consulting based on cognitive-behavioral treatment results in reduced anxiety in pregnant mothers who suffer from constipation. In the study of Bright et al. [88], online mental treatment resulted in reduced anxiety and improvement in the mental health of pregnant mothers.
Music and music therapy
Music therapy has a deep root in ancient Egypt, China, Rome, Greece, and India engravings, which consider music as a treatment essence with sedative effects. Music distracts the mind from the pain lower the intensity of the pain, creates muscle relaxation, and decreases the transmission of neural signals to the central nervous system. Among the mechanisms of music in decreasing pain, we can point out its activity in creating psychological and physiologic reactions, along with controlling sympathetic functions of the central nervous system, thereby reducing stress, emotions, and stimulation effect in people. Among the most important aspects of this method, choosing the type of music is critical. According to conducted studies, patients who choose music based on their preference experience lower heart rate, blood pressure, and anxiety level. Hence, the tempo of the music is effective in experiencing stress and anxiety. Accordingly, higher tempos make the mind more conscious and aware while slow music results in the sedation of the mind, improves the breath rhythm, lowers the heartbeat, and decreases stress [62]. In the study conducted by Toker et al. [89], listening to classic Turkish songs resulted in reduced anxiety and improved mental health of pregnant mothers with Pre-eclampsia. In the study conducted by Garcia and Gonazaks [90], music therapy resulted in reduced anxiety and improved growth parameters of fetus growth. In the study conducted by Aranzbetigon [91], music therapy programs along with mental imaging resulted in reduced anxiety and improved mental health of the mother along with enhancing the weight of the fetus with small for gestational age (SGA). In the review study conducted by Corbijen Wan and Wilsonford [92], music therapy and playing music resulted in reduced anxiety and stress in pregnant mothers. Nanbakhsh [93] found that music therapy resulted in reduced anxiety in mothers during the stages of childbirth.
Training during pregnancy and life skills teachings
Training during pregnancy can play a significant role in reducing illnesses and improving mental health during pregnancy and after childbirth. Training during pregnancy, particularly in groups and subgroups of high-risk pregnant women, is the most important preventive factor for mortality and also is crucial in lowering prenatal anxiety, depression, and mental disorders after childbirth and subsequent complications [26]. In the study conducted by Hoseini Nasab et al. [94], during-pregnancy training resulted in reduced anxiety during the stages of childbirth. Bogaerts et al. [95] found that training on changing lifestyle in obese pregnant women resulted in reduced anxiety and improved mental health and weighting of the pregnant mother during pregnancy. In the study conducted by Urizar [96], stress management programs resulted in reduced stress and anxiety along with decreased saliva cortisol hormone level in pregnant mothers. In the study conducted by Tragea et al. [35], stress management programs in 6 weeks resulted in reduced stress and anxiety in pregnant mothers. Urizar et al. [97] showed that stress management training programs resulted in reduced stress and anxiety in the cortisol hormone level in pregnant women with low income. The WHO has described life skills to strengthen and improve self-efficacy. They describe life skills as mental-social abilities necessary for adaptive and effective behaviors that enable individuals to face routine challenges and needs of everyday life. Training these skills results in personal and social growth and maintains human rights while preventing mental-social problems [98]. In the study conducted by Golshani et al. [98], training life skills results in reduced anxiety and improved mental health of pregnant women.
Combinatorial treatments
Combinatorial treatments that are common during pregnancy include plant therapy, reflexology, homeopathy and Chinese traditional medicine, pressure treatment, massage, yoga, aromatherapy, and bodily interventions. In the study conducted by Schijel [37], combinatorial treatments (pressure treatment, mental imaging, massage, reflexology, and relaxation) resulted in reduced anxiety while improving the mental health of high-risk pregnant women. Wang and Zehang [38] showed that using combinatorial treatment (pressure treatment, massage, physical training, vegan diet and vegan food, water therapy, mental support, and relaxation) resulted in reduced anxiety while improving the mental health of pregnant mothers during the COVID-19 pandemic. In the study conducted by Newham et al. [99], using combinatorial treatment resulted in reduced anxiety, while improving the mental health of pregnant women. In the study conducted by Javanbakht et al. [100], Satyapriya et al. [101], and Newham et al. [102], training and performing Yoga during pregnancy resulted in reduced anxiety and depression, while improving the mental health of pregnant women. van der Zwan et al. [103] found that performing biofeedback resulted in reduced anxiety while improving the mental health of pregnant women.
Reflexology has been used as a natural and old treatment method. It is believed that all organs and glands of the body are related to the reflexive points in the legs, hands, and ears. Experts in reflexology medicine believe that the foot is divided into numerous reflexive points that are related and adapted to all parts and organs of the body. Reflexology, as a complementary treatment, has been used from ancient times up to now and includes massaging the reflexive points in hands and feet that affect other parts of the body [104]. In the study conducted by Mirzaee et al [104], performing reflexology resulted in reduced anxiety during childbirth in pregnant mothers. Massage therapy is one the most common type of complementary treatments used in nursing and obstetric fields as its implementation is easy, safe, noninvasive, and comparatively inexpensive [105]. Bazrafshan and Ghorbani [105] found that performing massage based on superficial back strokes resulted in reduced anxiety in pregnant women.
Intimacy is a warm and sustained relationship between the mother and the child and facilitates the mother-child interaction. Intimacy is an emotional relationship that is formed during pregnancy and is enhanced after childbirth with eye-, smell-, and touch-contact relationships. The intimacy in the mother-fetus relationship plays a crucial role in the health of the pregnant mother and her fetus and is a vital factor in creating the mother’s identity while acting as a critical factor in the evolution of the child’s emotion [40]. In the study conducted by Rafiee et al. [40], training intimacy along with relaxation treatments resulted in reduced anxiety in pregnant women in their third quarter. Akbarzade et al. [25] showed that training in intimate behaviors and performing relaxation results in reduced anxiety in pregnant women. Castel et al. [106] found that training intimate behaviors in fathers and pregnant moths results in reduced anxiety. Other methods used in research that resulted in reduced anxiety included training with a pregnancy ball [107], performing KMC [108], performing sonography [109], supporting the pregnant mother in their third quarter [110], and chewing gum [111, 112].
Discussion
The present study was conducted to collect, analyze, and compare different effective and non-pharmacological methods in the reduction of anxiety in low-risk and high-risk pregnant women in Iran and worldwide from the beginning of 2000 to the end of 2022. To analyze these studies, we used the Jadad framework. Accordingly, studies that scored 3 or higher have sufficient quality. Most studies were conducted on low-risk pregnant women, and several studies (around 10) were done on high-risk pregnant women. A total of 23 different methods were used during pregnancy or in the first stages of pregnancy which resulted in the reduction of anxiety. Employing various methods of relaxation (20 studies), mindfulness (15 studies), using the sound of the Quran, and spiritual treatment based on religious training (14 studies) were among the most frequent methods reported by researchers. Among the studies conducted on the effect of relaxation on the reduction of anxiety in pregnant women, active relaxation and progressive muscle relaxation were used more frequently because they are more simple and understandable by pregnant women. It is essential to mention that in all the studies conducted, relaxation was performed as a method to reduce anxiety during pregnancy (not at the first stage of childbirth). Progressive muscle relaxation entails some training in which the individual flexes and releases the selected muscles until reaching deep relaxation. This process increases blood flow and then improves the muscle blood transfer function, thereby reducing muscle tension, stress, and anxiety [113]. In terms of mindfulness, in all the conducted research, mindfulness resulted in reduced anxiety during pregnancy (not at the first stage of childbirth). Regarding Quran verses and spiritual treatment based on religious training, these two methods were reported as effective and relaxing interventions in reducing anxiety during pregnancy and the first stage of childbirth. Obtaining a calm and satisfying state during pregnancy and then eventually giving birth to a healthy and righteous child while maintaining mental and spiritual calmness is in the light of the principles and guidelines of the holy Quran. Also, in high-risk pregnant women, the stronger their religious beliefs, the lower their experience of hopelessness and grief [57]. Training during pregnancy based on religious teachings increases the consciousness of pregnant mothers regarding preserving actions during pregnancy, childbirth and milking while reducing their anxiety [56-69]. In addition, consulting and religion-based psychotherapy can be used to reduce mental problems and enhance mental health. In religious-spiritual psychotherapy, strengthening the spiritual and religious beliefs of the individual, paying attention to the order of the universe, and the existence of the omnipotent God almighty results in a new cognition that is based on religious and Islamic training. Also, considering the vulnerability of pregnant women in terms of mental health, participating in spiritual-religious psychotherapies significantly reduces stress, anxiety, and depression [60]. It is essential to mention that considering that during pregnancy, the awareness of pregnant women regarding their diet, especially Halal food, the abundance and difference of food and drinks, prayings and self-realizing, remembering God for mental and spiritual sedation, having a sexual relationship in a proper framework without anxiety and stress is much higher, receiving support and care will undoubtedly be more. Considering the average awareness and positive viewpoint of most pregnant women and the undeniable force of religion on improving health, it is suggested that healthcare officials devise programs for providing pregnant women with care based on Islamic guidance, and the healthcare staff pay attention to this critical aspect more attentively [60].
Conclusion
A review of clinical trials conducted on different methods of reducing mothers’ anxiety during pregnancy has shown the numerous research on the field of relaxation, mindfulness, and the sound of Quran verses and spiritual treatment based on religious teachings. The results have shown that the use of active relaxation and progressive muscle relaxation can be a practical method to reduce anxiety and disorders during pregnancy due to being easy and understandable. Meanwhile, employing the sound of Quran verses and spiritual treatment based on religious training, considering Iranian and Islamic culture, as an effective method can play a vital role in this field. Considering that pregnancy and childbirth care is one of the most sensitive and critical services of the healthcare system worldwide, employing methods, such as religious training and awareness, improves the self-confidence and mental health of the individual, thereby improving the immunity system and helping pregnant women to face the anxiety of pregnancy and pass the pregnancy and childbirth. Also, considering that in high-risk pregnant women, the rate of anxiety disorders, isolation, and problems in personal, familial, and social life is higher, these two methods, due to being easy to understand and simple, can significantly affect mothers and improve their adaptability to pregnancy.
Ethical Considerations
Compliance with ethical guidelines
This article is a meta-analysis with no human or animal sample.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed equally in preparing all parts of the research.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
We thank the support and cooperation of officials at the department of nursing and obstetrics, the library, and the computer center of the Azad Islamic university, Najaf Abad branch, for performing the search and conducting this study.
References
Based on the reports provided by the World Health Organization (WHO), behavioral illnesses are the second cause of disability worldwide [1]. Mental health issues affect all societies and age groups, among which pregnant women are not an exception [2]. The mental health of the pregnant mother during pregnancy is influenced by hormonal changes and in women who consider pregnancy as a completely biological process, this is considerably joyful and gratifying. However, many women experience anxiety during this period because, during pregnancy, the individual faces major changes in their lifestyle and should create alterations in their self-image and get prepared for motherhood [3]. Based on the reported systematic reviews, mental disorders, such as depression and anxiety in women during pregnancy are more prevalent in women in low- to medium-income countries [4]. Also, the point-to-point prevalence of mental disorders during pregnancy has been reported at 14%, of which 3.3% are related to acute depression and 6.6% are related to anxiety disorders [3].
More than 50% of women experience various levels of anxiety during pregnancy, among which 8.5% to 10.5% are related to anxiety, 1.45% to 5.2% are related to fear, 1.2% to 5.1% are related to obsession and 0.3% are related to posttraumatic stress disorder [5]. Based on previous research, anxiety has been reported in 15% of Iranian pregnant women [6]. Some of the pre-existing conditions that create anxiety disorders and changes in the mental health of pregnant women are age, first-child pregnancy, physical disorders and illness, heredity, and mother-born anxiety [7], hormonal changes [8], the experience of premature childbirth and mother whose child are at great risk of abnormalities [3].
Anxiety during depression can directly affect the pattern of fetus growth and the length of pregnancy [9], or it may have significant implications, including low-weight childbirth and low Apgar score [10]. Anxiety also creates the discharge of stress hormones (adrenal steroids and corticotropin-releasing hormone) that these hormones affect the growth of the fetus’s brain growth in weeks 12 to 22 by passing the pair [11] and play a major role in premature childbirth [12]. Additionally, these hormones can cause paired vasoconstriction and limit oxygen and nutrition transfer to the fetus [11]. Meanwhile, researchers believe that stress and anxiety during pregnancy can cause vascular blood pressure and reduce the blood flow of fetus-pair while increasing the resistance of paired vessels [13]. All these factors can be the reasons for the limitation of fetus growth and fetal asphyxia [14].
In previously conducted studies, cortisol (among the stress hormones) is defined as one of the limiting factors of fetus growth [15]. High levels of anxiety in mothers and an increase in the level of cortisol hormone in amniotic fluid can affect the evolutionary process of the fetus’ brain along with social skills, communication power, and child memory in the future. Based on reports, around 15% of issues in delayed recognition and anxiety in children are the result of anxiety in the mother during pregnancy [16, 17]. The abnormal status of mental health in a pregnant woman and the existence of severe and constant anxiety cause the fetus to be exposed to glucocorticoids for a longer time and this causes constant neuroendocrine alterations in the individual. These changes can cause particular cognition or behavioral patterns and result in future problems in controlling emotions or character shocks in the fetus [18]. The study by O’Connor et al. has shown that the abnormal mental health of the mother in the 32nd week of pregnancy can cause behavioral and emotional disorders in the child up until the age of 7 years, and bring the craving symptoms in pregnant women to an uncontrollable level [19]. On the other hand, it should be noted that 20% of pregnancies can be classified as high-risk pregnancies [20]. The rate of pregnant women in the high-risk group who required special care equals 76.6% [21].
High-risk pregnant women face dangers and problems in their personal, familial, and social life and a high-risk pregnancy affects the individual and results in changes in the family functions. Evidence suggests that in high-risk pregnant women, the rate of depression is 44%, major depression 19% [22], increased rates of psychosis, anxiety, mental disorders, isolation, consumption, and sleep disorders, and fear of illness and loneliness are higher during pregnancy and after childbirth [23]. Also, in high-risk pregnant women, the possibility of the occurrence of behavioral problems is higher in their children [24]. Numerous studies have suggested nursing and obstetrics techniques as alternative treatment methods to improve mental health and reduce anxiety in pregnant women, including relaxation [9, 13-15, 25-40], mindfulness [41-55], Quran verses and spiritual treatment based on religious training [56-69], aromatherapy [70-80], consulting, spouse support and behavioral and cognition treatments [81-88] music therapy [62, 89-93], training during pregnancy and life skills [26, 35, 94-98], complementary treatments [25, 37, 38, 40, 99-106], pregnancy ball [107], KMC [108], sonography [109], supporting and accompanying pregnant mothers in the third month of school [110] and chewing gum [111, 112] .
Considering the importance of adverse effects of anxiety in pregnant women, especially high-risk pregnant women, and given the numerous studies conducted on different methods of reducing anxiety in pregnant mothers and discrepancies in the results and the lack of review studies in this field in Iran, this study aims to conduct a systematic review of conducted studies to present the best and most effective non-pharmacological methods to reduce anxiety in pregnant women at low-risk and high-risk levels in Iran and worldwide.
Materials and Methods
In this systematic review, we used all the conducted clinical trials on various types of effective non-pharmacological methods in reducing the anxiety of pregnant women in both low-risk and high-risk groups in Iran and worldwide from the beginning of 2000 to the end of 2022. The method of presenting the materials, including defining the subject, data collection, and analysis of the results, was conducted based on the PRISMA framework. To conduct the electronic search, we used time limitations. Accordingly, all published articles from the beginning of 2000 to the end of 2022 were investigated. To reach the required information from the published articles in national journals, databases of IRCT, Scopus, Irandoc, MEDLIB, Google Scholar, SID, and other articles were searched on PubMed, Science Direct, and Cochrane.
To maximize the generalizability of the search in Persian references, general and specific keywords were used as follows, anxiety, pregnancy, childbirth, mother, high-risk, clinical trial, low-risk, non-pharmacological, and their possible combinations in the abstract, title, and keywords. Accordingly, we used the operators “AND” and “OR”. For English databases the following equivalents and MeSH words were employed, “anxiety”, “pregnancy”, “delivery”, “childbirth”, “mother”, “clinical trial”, “high risk”, “low-risk”, and “non-drug”. We used the operators of “AND” and “OR” for combinatorial search. In the Google Scholar database, the keywords were entered into the subject field and all resulting articles were investigated. The inclusion criteria included being a clinical trial study and employing a method to reduce anxiety during pregnancy or childbirth in women in both groups low-risk and high-risk. To evaluate articles, we used the Jadad framework.
Results
In this systematic review, a total of 120 articles were investigated. Among the investigated articles, 99 papers (52 Persian and 47 English) were selected for review. A total of 10 articles were related to high-risk pregnant women and 89 articles were conducted on low-risk pregnant women. A total of 23 different treatment methods were used to reduce anxiety in pregnant women with low-risk and high-risk during pregnancy and or the first stage of childbirth (Figure 1). In some of these studies, other variables are investigated at the same time as analyzing anxiety in pregnant women. For instance, in terms of improving the parameters of the fetus growth, 4 articles, in terms on reducing depression, 20 articles, on reducing stress, 19 articles, on improving mental health, 18 articles, on improving quality of life, 1 article, on improving sleep quality, 2 articles, and in terms of cortisol hormone level, 4 articles were conducted. Based on the investigations, the effect of relaxation (20 articles), mindfulness (15 articles), Quran verses and spiritual-based treatment based on religious training (14 articles), and aromatherapy (11 articles) along with music therapy (6 articles) were among the most frequent treatment methods in studies investigated by researchers, compared to other methods. All these methods are briefly explored in the following (Table 1).



Relaxation
Among the most common relaxation methods were progressive muscle relaxation (Jacobsen), passive relaxation, Benson relaxation, mental relaxation (Mitchel), conscious breathing, mental imaging, the method of teaching the self, and a combination of various methods. In most articles regarding the use of relaxation as an intervention, progressive muscle relaxation was employed the most. This method was designed by Edmon Jacobsen and is among the active muscle-mind relaxation methods. In muscle-mind techniques, by flexing and releasing the muscle, various parts of the body become the focus of the mind and then they are rested. In this method, the mind learns to focus on different parts of the body and remove the outside world while experiencing freeness, thereby gaining serenity. By flexing and resting the muscle, this method changes the focus of the mind from the external world to the internal world. Also, in this method, the flexing and relaxing process can be done in separation (the muscle of the tow, then the muscle of the fingers, and then the muscle of the calves, next the muscles of the thighs, etc.), in the group (multiple muscles together, for instance, the muscles of the calves and thighs, etc.), or even one half of the body (all muscles of the right side of the body and next the left side [26].
A total of 20 articles were conducted on the effect of relaxation on anxiety during pregnancy and 18 articles concluded that performing relaxation practices results in the reduction of anxiety during pregnancy [9, 13-15, 25-40] and in two articles, the reduction in anxiety during pregnancy was not reported [32, 33]. In the study by Brigstom et al. conducted in 2009 [32], performing passive relaxation did not result in stress and anxiety reduction during pregnancy, enhanced experience of pregnancy, and reduced Epidural anesthesia. In the study conducted by Gidy Dahel and Forse [33], performing relaxation did not result in reduced anxiety during pregnancy or reduced pregnancy pain and improved Apgar score. It is essential to mention that these two articles were performed on high-risk pregnant women. In the study conducted by Rahimi et al. [26], performing progressive muscle relaxations resulted in reduced anxiety in high-risk pregnant women. In the study conducted by Schiljel et al [37], performing combinatory treatments and relaxation treatments resulted in reduced anxiety in high-risk pregnant women. In addition, in the study conducted by Wang and Zahang [38], performing combinatory treatment and relaxation practice resulted in reduced anxiety and improved mental health during the COVID-19 pandemic. In the study conducted by Rafiee et al. [40], performing relaxation treatment along with intimacy training resulted in reduced anxiety in pregnant women in their third quarter.
Mindfulness
Mindfulness is an objective awareness that cannot be described and is based on the present time in terms of the experience in a particular moment in the attention span of the individual. In addition, this notion includes the confession of a remembered experience and its acceptance. In another description, mindfulness is described as a technique that along with meditation and particular mind orientations toward an experience promotes objective awareness of the present while minimizing the entanglement of thoughts and emotions [56]. Mindfulness is performed for patients to convince them that thoughts are merely thoughts and they are not reality. When they can consider their thoughts as they are and as an external phenomenon, they can view reality more clearly and manage their affairs more effectively. Mindful individuals comprehend internal and external reality more freely and without distortion and have the ability to face a wide range of thoughts, emotions, and pleasant or unpleasant experiences [53]. A total of 15 articles were conducted on the effect of mindfulness on the anxiety level in pregnant women, and all these articles concluded that mindfulness can decrease anxiety during pregnancy [41-55]. Maren Goetz et al. [51] showed that performing electronic mindfulness for a week resulted in reduced anxiety in high-risk pregnant mothers. In some of these studies, other variables, along with studying the effect of mindfulness on the anxiety of pregnant women, have been investigated, including the reduction of depression in 11 articles [41-45, 47-52], improvement in sleep quality of pregnant women in 2 studies [45, 52], the reduction of cortisol hormone in 1 article [45], the reduction of changes in the blood pressure of pregnant women in 1 article [45], the reduction of stress in pregnant women in 8 articles [41-45, 47-52], improvement in the mental health of the mothers and fathers during pregnancy in 1 article [46], enhancing self-efficacy in milking for mother in 1 article [48], and improving infant growth parameters in the article [53].
Quran verses and religious beliefs
Religious beliefs improve health, quality of life, and dependence on God. In the conducted investigations, the positive effect of religion has been reported, for instance, in women who had experienced a high-risk pregnancy. Since the religious beliefs were stronger in these individuals, hopelessness and grief were reported at lower levels [57]. In the study conducted by Niaz Azari et al. [58], group spiritual treatment in diabetic pregnant women resulted in reduced anxiety and improved quality of life. Religious beliefs and prayers positively affect the mental and physical health of the individual [57, 59]. Treatment with beliefs and faith in God for improvement is among the methods that are based on psychology and have great importance in treating illnesses and reducing pain, anxiety, and depression [57]. In the study conducted by Bodaghi et al. [59], increasing levels of spirituality in pregnant women resulted in reduced stress, anxiety, and depression in mothers. Azizi et al. [60] reported the effectiveness of religious training in the reduction of anxiety in pregnant women. Khodakarami et al. [61] indicated that spiritual-based consulting during pregnancy results in reduced stress, anxiety, and depression in mothers. Therefore, considering that pregnancy and childbirth is a sensitive period in an individual’s life, improving religious beliefs and faith can be sedative and help in the health of the mother and the baby. It is emphasized that society officials and religious leaders should participate in health promotion programs for pregnant women [57].
Quran verses
The Quran, the holy book of Muslims, considers all aspects of life, and reading it is similar to spiritual music that helps in releasing endorphins by stimulating the brain’s alpha waves. Accordingly, reading the Quran helps to eliminate negative emotions and create serenity, and strengthen the stress threshold in an individual [62]. The sound of the Quran has eloquent, simple, and elegant music that if these characteristics become available, hearers from different groups will be affected by it and their bodies and soul will be captured by it. Listening to the Quran is a systematic and complementary therapy that can help reduce stress and improve critical life symptoms [61]. In a study conducted by Naderyanfar et al. [63], listening to the Quran resulted in reduced anxiety in mothers volunteering for natural childbirth. In the review study conducted by Irani et al. [62], the sound of reading the Quran was a considerably effective factor in reducing anxiety and pain in mothers during childbirth. Employing this method has various benefits, such as less time consumption, easy access, inexpensive, noninvasive, and no danger for the patient, compared to pharmacological treatments. Abbasi et al. [64] indicated that reading the translation of Yasin Surah for 15 days results in reduced anxiety in women in their second and third quarters. Sahmeddini et al. [65] showed that listening to the sound of the Quran with headphones for 45 minutes in a maternity hospital resulted in reduced anxiety in pregnant women along with decreased serum levels of cortisol hormone. In a study conducted by Kadkhodaei et al. [66], listening to Quran sounds results in reduced anxiety in pregnant women. In the study conducted by Fitri et al. [67], listening and reading Al-Rahman Surah for 15 minutes, three times a week in the third quarter of pregnancy resulted in reduced anxiety in Indonesian pregnant women. Sohita and Mofidah [68] found that reciting Al-Rahman Surah in the active stage of pregnancy resulted in reduced anxiety and pregnancy pain in Indonesian pregnant women. In the study conducted by Mirbagher Ajorpaz and Ranjbar [69], listening to the sound of the Quran resulted in reduced anxiety in pregnant women candidates for cesarean.
Aromatherapy
Aromatherapy is a combinatory treatment method that with the help of fragrant smells and stimulating the olfactory sense results in sedation with the release of endorphins and reduces pain and anxiety [70, 71]. In addition, aromatherapy affects the hypothalamus by stimulating the olfactory sense and reduces the release of corticotropin that subsequently decreases the release of Adrenocorticotropic hormone from the hypophysis and then lowers the release of cortisol from the adrenal gland, thereby reducing anxiety [71]. In various studies, different essences have been employed. In a study conducted by Mirzae et al [72], smelling lavender resulted in reduced cortisol hormone and anxiety while increasing the level of serotonin hormone during pregnancy. In the study of Tafazoli et al., smelling lavender [73], in the study by Namazi et al., the smell of orange blossoms [70], in the study by Ozgoli et al., the smell of peppermint and clove [71], in the study of Kheirkhah et al., the smell of damask rose with hot shower [74], in the study of Sharifipour et al., the smell of common sage [75], in the study of Ozgoli et al., the smell of peppermint [76], in the study of Esmaelzadeh et al., the smell of Boswellia [77], in the study of Hamedanian et al., smelling rose [78], in the study of Rashidi Fakar et al., the smell of geraniums [79], and in the study of Rashidi Fakari et al., the smell of orange essence [80] have been reported to reduce the anxiety of pregnant mothers.
Consulting, support of the spouse, and cognitive behavioral treatments
The principles of consulting are based on listening and trying to understand the viewpoints and worries of the mother, respecting her, and trying to maintain a sympathetic and positive relationship with her [81]. In the study conducted by Moghadasi et al [81], performing support consulting resulted in reduced anxiety in mothers along with mothers who were exposed to the risk of premature childbirth. The obstetrician, as responsible, plays a crucial role in providing consultancy and care for the pregnant mother [82]. Andaroon et al. [82] showed that performing individual consulting by the obstetrician resulted in reduced anxiety in mothers during pregnancy. Consulting the pregnant mother with the spouse in terms of spiritual and mental support for the mother during pregnancy can reduce the anxiety and worries of pregnant women during pregnancy, thereby resulting in a healthier and more dynamic society with mentally and physically healthy children [83]. In the study conducted by Barjaste and Moghadam [83], performing couple consultations based on the support of the spouse resulted in reduced anxiety and worries of the pregnant mother. In the study conducted by Mohammadpour et al. [84], performing spouse consulting resulted in reduced anxiety in mothers during pregnancy.
In cognitive-behavioral treatments, individuals distance themselves from negative thoughts and try to participate in activities and obtain dominance, thereby resulting in the reduction of anxiety [85]. In the study conducted by Imanparast et al. [85], performing cognitive-behavioral treatments results in reduced anxiety in mothers. In the study conducted by Mationecsicar [86], performing positive cognitive-behavioral intervention results in reduced anxiety and stress while improving the mental health status of pregnant mothers. In the study conducted by Ghorbani et al. [87], performing group consulting based on cognitive-behavioral treatment results in reduced anxiety in pregnant mothers who suffer from constipation. In the study of Bright et al. [88], online mental treatment resulted in reduced anxiety and improvement in the mental health of pregnant mothers.
Music and music therapy
Music therapy has a deep root in ancient Egypt, China, Rome, Greece, and India engravings, which consider music as a treatment essence with sedative effects. Music distracts the mind from the pain lower the intensity of the pain, creates muscle relaxation, and decreases the transmission of neural signals to the central nervous system. Among the mechanisms of music in decreasing pain, we can point out its activity in creating psychological and physiologic reactions, along with controlling sympathetic functions of the central nervous system, thereby reducing stress, emotions, and stimulation effect in people. Among the most important aspects of this method, choosing the type of music is critical. According to conducted studies, patients who choose music based on their preference experience lower heart rate, blood pressure, and anxiety level. Hence, the tempo of the music is effective in experiencing stress and anxiety. Accordingly, higher tempos make the mind more conscious and aware while slow music results in the sedation of the mind, improves the breath rhythm, lowers the heartbeat, and decreases stress [62]. In the study conducted by Toker et al. [89], listening to classic Turkish songs resulted in reduced anxiety and improved mental health of pregnant mothers with Pre-eclampsia. In the study conducted by Garcia and Gonazaks [90], music therapy resulted in reduced anxiety and improved growth parameters of fetus growth. In the study conducted by Aranzbetigon [91], music therapy programs along with mental imaging resulted in reduced anxiety and improved mental health of the mother along with enhancing the weight of the fetus with small for gestational age (SGA). In the review study conducted by Corbijen Wan and Wilsonford [92], music therapy and playing music resulted in reduced anxiety and stress in pregnant mothers. Nanbakhsh [93] found that music therapy resulted in reduced anxiety in mothers during the stages of childbirth.
Training during pregnancy and life skills teachings
Training during pregnancy can play a significant role in reducing illnesses and improving mental health during pregnancy and after childbirth. Training during pregnancy, particularly in groups and subgroups of high-risk pregnant women, is the most important preventive factor for mortality and also is crucial in lowering prenatal anxiety, depression, and mental disorders after childbirth and subsequent complications [26]. In the study conducted by Hoseini Nasab et al. [94], during-pregnancy training resulted in reduced anxiety during the stages of childbirth. Bogaerts et al. [95] found that training on changing lifestyle in obese pregnant women resulted in reduced anxiety and improved mental health and weighting of the pregnant mother during pregnancy. In the study conducted by Urizar [96], stress management programs resulted in reduced stress and anxiety along with decreased saliva cortisol hormone level in pregnant mothers. In the study conducted by Tragea et al. [35], stress management programs in 6 weeks resulted in reduced stress and anxiety in pregnant mothers. Urizar et al. [97] showed that stress management training programs resulted in reduced stress and anxiety in the cortisol hormone level in pregnant women with low income. The WHO has described life skills to strengthen and improve self-efficacy. They describe life skills as mental-social abilities necessary for adaptive and effective behaviors that enable individuals to face routine challenges and needs of everyday life. Training these skills results in personal and social growth and maintains human rights while preventing mental-social problems [98]. In the study conducted by Golshani et al. [98], training life skills results in reduced anxiety and improved mental health of pregnant women.
Combinatorial treatments
Combinatorial treatments that are common during pregnancy include plant therapy, reflexology, homeopathy and Chinese traditional medicine, pressure treatment, massage, yoga, aromatherapy, and bodily interventions. In the study conducted by Schijel [37], combinatorial treatments (pressure treatment, mental imaging, massage, reflexology, and relaxation) resulted in reduced anxiety while improving the mental health of high-risk pregnant women. Wang and Zehang [38] showed that using combinatorial treatment (pressure treatment, massage, physical training, vegan diet and vegan food, water therapy, mental support, and relaxation) resulted in reduced anxiety while improving the mental health of pregnant mothers during the COVID-19 pandemic. In the study conducted by Newham et al. [99], using combinatorial treatment resulted in reduced anxiety, while improving the mental health of pregnant women. In the study conducted by Javanbakht et al. [100], Satyapriya et al. [101], and Newham et al. [102], training and performing Yoga during pregnancy resulted in reduced anxiety and depression, while improving the mental health of pregnant women. van der Zwan et al. [103] found that performing biofeedback resulted in reduced anxiety while improving the mental health of pregnant women.
Reflexology has been used as a natural and old treatment method. It is believed that all organs and glands of the body are related to the reflexive points in the legs, hands, and ears. Experts in reflexology medicine believe that the foot is divided into numerous reflexive points that are related and adapted to all parts and organs of the body. Reflexology, as a complementary treatment, has been used from ancient times up to now and includes massaging the reflexive points in hands and feet that affect other parts of the body [104]. In the study conducted by Mirzaee et al [104], performing reflexology resulted in reduced anxiety during childbirth in pregnant mothers. Massage therapy is one the most common type of complementary treatments used in nursing and obstetric fields as its implementation is easy, safe, noninvasive, and comparatively inexpensive [105]. Bazrafshan and Ghorbani [105] found that performing massage based on superficial back strokes resulted in reduced anxiety in pregnant women.
Intimacy is a warm and sustained relationship between the mother and the child and facilitates the mother-child interaction. Intimacy is an emotional relationship that is formed during pregnancy and is enhanced after childbirth with eye-, smell-, and touch-contact relationships. The intimacy in the mother-fetus relationship plays a crucial role in the health of the pregnant mother and her fetus and is a vital factor in creating the mother’s identity while acting as a critical factor in the evolution of the child’s emotion [40]. In the study conducted by Rafiee et al. [40], training intimacy along with relaxation treatments resulted in reduced anxiety in pregnant women in their third quarter. Akbarzade et al. [25] showed that training in intimate behaviors and performing relaxation results in reduced anxiety in pregnant women. Castel et al. [106] found that training intimate behaviors in fathers and pregnant moths results in reduced anxiety. Other methods used in research that resulted in reduced anxiety included training with a pregnancy ball [107], performing KMC [108], performing sonography [109], supporting the pregnant mother in their third quarter [110], and chewing gum [111, 112].
Discussion
The present study was conducted to collect, analyze, and compare different effective and non-pharmacological methods in the reduction of anxiety in low-risk and high-risk pregnant women in Iran and worldwide from the beginning of 2000 to the end of 2022. To analyze these studies, we used the Jadad framework. Accordingly, studies that scored 3 or higher have sufficient quality. Most studies were conducted on low-risk pregnant women, and several studies (around 10) were done on high-risk pregnant women. A total of 23 different methods were used during pregnancy or in the first stages of pregnancy which resulted in the reduction of anxiety. Employing various methods of relaxation (20 studies), mindfulness (15 studies), using the sound of the Quran, and spiritual treatment based on religious training (14 studies) were among the most frequent methods reported by researchers. Among the studies conducted on the effect of relaxation on the reduction of anxiety in pregnant women, active relaxation and progressive muscle relaxation were used more frequently because they are more simple and understandable by pregnant women. It is essential to mention that in all the studies conducted, relaxation was performed as a method to reduce anxiety during pregnancy (not at the first stage of childbirth). Progressive muscle relaxation entails some training in which the individual flexes and releases the selected muscles until reaching deep relaxation. This process increases blood flow and then improves the muscle blood transfer function, thereby reducing muscle tension, stress, and anxiety [113]. In terms of mindfulness, in all the conducted research, mindfulness resulted in reduced anxiety during pregnancy (not at the first stage of childbirth). Regarding Quran verses and spiritual treatment based on religious training, these two methods were reported as effective and relaxing interventions in reducing anxiety during pregnancy and the first stage of childbirth. Obtaining a calm and satisfying state during pregnancy and then eventually giving birth to a healthy and righteous child while maintaining mental and spiritual calmness is in the light of the principles and guidelines of the holy Quran. Also, in high-risk pregnant women, the stronger their religious beliefs, the lower their experience of hopelessness and grief [57]. Training during pregnancy based on religious teachings increases the consciousness of pregnant mothers regarding preserving actions during pregnancy, childbirth and milking while reducing their anxiety [56-69]. In addition, consulting and religion-based psychotherapy can be used to reduce mental problems and enhance mental health. In religious-spiritual psychotherapy, strengthening the spiritual and religious beliefs of the individual, paying attention to the order of the universe, and the existence of the omnipotent God almighty results in a new cognition that is based on religious and Islamic training. Also, considering the vulnerability of pregnant women in terms of mental health, participating in spiritual-religious psychotherapies significantly reduces stress, anxiety, and depression [60]. It is essential to mention that considering that during pregnancy, the awareness of pregnant women regarding their diet, especially Halal food, the abundance and difference of food and drinks, prayings and self-realizing, remembering God for mental and spiritual sedation, having a sexual relationship in a proper framework without anxiety and stress is much higher, receiving support and care will undoubtedly be more. Considering the average awareness and positive viewpoint of most pregnant women and the undeniable force of religion on improving health, it is suggested that healthcare officials devise programs for providing pregnant women with care based on Islamic guidance, and the healthcare staff pay attention to this critical aspect more attentively [60].
Conclusion
A review of clinical trials conducted on different methods of reducing mothers’ anxiety during pregnancy has shown the numerous research on the field of relaxation, mindfulness, and the sound of Quran verses and spiritual treatment based on religious teachings. The results have shown that the use of active relaxation and progressive muscle relaxation can be a practical method to reduce anxiety and disorders during pregnancy due to being easy and understandable. Meanwhile, employing the sound of Quran verses and spiritual treatment based on religious training, considering Iranian and Islamic culture, as an effective method can play a vital role in this field. Considering that pregnancy and childbirth care is one of the most sensitive and critical services of the healthcare system worldwide, employing methods, such as religious training and awareness, improves the self-confidence and mental health of the individual, thereby improving the immunity system and helping pregnant women to face the anxiety of pregnancy and pass the pregnancy and childbirth. Also, considering that in high-risk pregnant women, the rate of anxiety disorders, isolation, and problems in personal, familial, and social life is higher, these two methods, due to being easy to understand and simple, can significantly affect mothers and improve their adaptability to pregnancy.
Ethical Considerations
Compliance with ethical guidelines
This article is a meta-analysis with no human or animal sample.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
All authors contributed equally in preparing all parts of the research.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
We thank the support and cooperation of officials at the department of nursing and obstetrics, the library, and the computer center of the Azad Islamic university, Najaf Abad branch, for performing the search and conducting this study.
References
- Murry CJL, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global burden of disease study. Lancet. 1997; 349(9064):1498-504. [DOI:10.1016/S0140-6736(96)07492-2] [PMID]
- O’Connor TG, Ben-Shlomo Y, Heron J, Golding J, Adams D, Glover V. Prenatal anxiety predicts individual differences in cortisol in pre-adolescent children. Biological Psychiatry. 2005; 58(3):211-7. [DOI:10.1016/j.biopsych.2005.03.032] [PMID]
- Leveno KJ, Spong CY, Dashe JS, Casey BM, Hoffman BL, CunninghamFG, et al. Williams obstetrics. 25th ed. New york: MCGraw-Hill; 2018. [Link]
- López-Morales H, del Valle M, Canet-Juric L, Andrés M, Galli J, Poó F, et al. Mental health of pregnant women during the COVID-19 pandemic: A longitudinal study. Psychiatry Research. 2021; 295:113567. [DOI:10.1016/j.psychres.2020.113567] [PMID] [PMCID]
- Avni-Barron O,Wiegartz PS. Issues in treating anxiety disorder in pregnancy. Understanding the causes to make better treatment Decisions. Psychiatr Times. 2011; 28(1):47-50. [Link]
- Janati Y, Khaki N. [Psychiatric in midwifery (Persian)]. Tehran: Jame Negar; 2005. [Link]
- Adewuya AO, Ola BA, Aloba OO, Mapayi BM. Anxiet disorders among Nigeria women in late pregnancy: A controlled study. Archives of Women's Mental Health. 2006; 9(6):325-8. [DOI:10.1007/s00737-006-0157-5] [PMID]
- Smith SS, Shen H, Gong QH, Zhou X. Neurosteroid regulation of GABA(A) receptors: Focus on the alpha4 and delta subunits. Pharmacology & Therapeutics. 2007; 116(1):58-76. [DOI:10.1016/j.pharmthera.2007.03.008] [PMID] [PMCID]
- Fink N, Urech C, Cavelti M, Alder J. Relaxation during pregnancy: What are the benefits for mother, fetus, and the newborn? A systematic review of the literature. The Journal of Perinatal & Neonatal Nursing. 2012; 26(4):296-306. [DOI:10.1097/JPN.0b013e31823f565b] [PMID]
- Warren SL, Racu C, Gregg V, Simmens SJ. Maternal paniv disorder: infant prematurity and low birth weight. Journal of Anxiety Disorders. 2006; 20(3):342-52. [DOI:10.1016/j.janxdis.2005.02.007] [PMID]
- Weinstock M. The long-term behavioral consequences of prenatal stress. Neuroscience and Biobehavioral Reviews. 2008; 32(6):1073-86. [DOI:10.1016/j.neubiorev.2008.03.002] [PMID]
- Shahhosseni Z, Abedian K, Azimi H. [Anxiety during pregnancy in preterm delivery (Persian)]. Journal of Advances in Medical and Biomedical Research. 2007; 16(63):85-92. [Link]
- Urech C, Fink NS, Hoesli I, Wilhelm FH, Bitzer J, Alder J. Effect of relaxation on psychobiological wellbeing during pregnancy: A randomized controlled trial. Psychoneuroendocrinology. 2010; 35(9):1348-55. [DOI:10.1016/j.psyneuen.2010.03.008] [PMID]
- Alipoor Z, Lamyianm M, Hajizade E. [Anxiety in pregnancy: Risk for outcome child birth (Persian)]. Journal of Urmia Nursing and Midwifery Faculty. 2009; 9(1):30-8. [Link]
- Teixeira J, Martin D, Prendiville O, Glover V. Theeffects of acute relaxation on indices of anxiety during pregnancy. Journal of Psychosomatic Obstetrics and Gynaecology. 2005; 26(4):271-6. [DOI:10.1080/01674820500139922] [PMID]
- Okour AM, Badarneh R. Spousal violence against pregnant women from a Bedouin Community in Jordan. Journal of Women's Health. 2011; 20(12):1853-9. [DOI:10.1089/jwh.2010.2588] [PMID]
- Brownridge DA, Taillieu TL, Tyler KA, Tiwari A, Ko ling CH, Santos SC. Pregnancyand intimate partner violence: Risk factors, severty, and health effects. Violence Against Women. 2011; 17(7):858-81. [DOI:10.1177/1077801211412547] [PMID]
- Van den Bergh BR, Mulder EJ, Mennes M, Glover V. Antenatal maternal anxiety and stress and neurobehavioural development of the fetus and child: links and possible mechanisms. A review.Neuroscience and Biobehavioral Reviews. 2005; 29(2):237-58. [DOI:10.1016/j.neubiorev.2004.10.007] [PMID]
- Swallow BL, Lindow SW, Masson EA, Hay DM. Psychological health in early pregnancy: Relationship with nausea and vomiting. Journal of Obstetrics and Gynaecology . 2004; 24(1):28-32. [DOI:10.1080/01443610310001620251] [PMID]
- James DK, Steer PJ, Weiner CP, Gonik B. High risk pregnancy e-book: Management options-expert consult. London: Elsevier Health Sciences; 2010. [Link]
- Ministry of Health and Medical Education. [Manual nationalsafe motherhood program(instruction integrated maternal healthcare) GP and mamae specially maternal health Administration, Bureau of Family Health and Population (Persian)]. Tehran: Ministry of Health and Medical Education; 2017.
- Rayegan R, KHodakarami N, Hasanzade M, Akbarzade. [Assessing the mental health of mothers with high-risk and low-risk pregnancies (Persian)]. Scientific Journal of the Medical System Organization of the Islamic Republic of Iran. 2012; 30(4):329-34. [Link]
- Akbarzade M. [Mental health in pregnancy & child birth (Persian)]. Tehran: Hydari publishers; 2012. [Link]
- Heron J, O’ConnorTG, EvansJ, GoldingJ, Glover V, ALSPAC Study Team. The course of anxiety and depression through pregnancy and the postpartum in a community sample. Journal of Affective Disorders. 2004; 80(1):65-73. [DOI:10.1016/j.jad.2003.08.004] [PMID]
- Akbarzade M, ToosiM, Zare N, Sharif F. [Effect of Relaxation and attachment behaviors training on anxiety in first-time mothers in shiraz city: A randomized clinical trial (Persian)]. Qom University of Medical Sciences Journal. 2013; 6(4):14-23. [Link]
- Rahimi F, Ahmadi M, Rosta F, Alavi Majd H, Valiani M. [Effect of relaxation training on pregnancy anxiety in high risk women (Persian)]. Safety Promotion and Injury Prevention. 2014; 2(3):180-8. [doi:10.22037/meipm.v2i3.7737]
- Alder J, Urech C, Fink N, Bitzer J, Hoesli I. Response to Induced relaxation during pregnancy: Comparison of women with high versus low levels of anxiety. Journal of Clinical Psychology in Medical Settings. 2011; 18(1):13-21. [DOI:10.1007/s10880-010-9218-z] [PMID]
- Bastani F, Hidarnia A, Kazemnejad A, Vafaei M, Kashaian M. A randomized controlled trial of the effects of applied relaxation training on reducing anxiety and perceived stress in pregnant women. Journal of Midwifery & Women's Health. 2005; 50(4):e36-40. [DOI:10.1016/j.jmwh.2004.11.008] [PMID]
- Nasiri S, Akbari H, Tagharrobi L, Tabatabaee AS. The effect of progressive muscle relaxation and guided imagery on stress, anxiety, and depression of pregnant women referred to health centers. Journal of Education and Health Promotion. 2018; 7:41. [doi:10.4103/jehp.jehp_158_16]
- Ahmadi Nejad F, Golmakani N, Asghari Pour N, Shakeri M. [Effect of progressive muscle relaxation on depression, anxiety, and stress of primigravid women (Persian)]. Evidence Based Care Journal. 2015; 5(1):67-75. [doi:10.22038/ebcj.2015.4093]
- Yu J, Wells J, Wei Z, Fewtrell M. Effects of relaxation therapy on maternalpsychological state, infant growth and gutmicrobiome: Protocol for a randomisedcontrolled trial investigating mother-infantsignalling during lactation following latepreterm and early term delivery. International Breastfeeding Journal . 2019; 14:50. [DOI:10.1186/s13006-019-0246-5] [PMID] [PMCID]
- Bergstrom M, Kieler H, Waldenstrom U. Effect of natural childbirth preparation versus standard antenatal education on epidural rates ,experience of childbirth and parental stress in mothers and fathers: A randomized controlled multicenter trial. BJOG an International Journal of Obstetrics and Gynaecology. 2009; 116(9):1167-76. [DOI:10.1111/j.1471-0528.2009.02144.x] [PMID] [PMCID]
- Gedde-Dahl M, Fors EA. Impact of self-administered relaxation and guided imagery techniques during final trimester and birth.Complementary Therapies in Clinical Practice. 2012; 18(1):60-5. [DOI:10.1016/j.ctcp.2011.08.008] [PMID]
- Fotiou C, Vlastarakos PV, Bakoula C, Papagaroufalis K, Bakoyannis G, Darviri C, et al. Parental stress management using relaxation techniques in a neonatal intensive care unit: A randomised controlled trial. Intensive & Critical Care Nursing. 2016; 32:20-8. [DOI:10.1016/j.iccn.2015.08.006] [PMID]
- Tragea C, Chrousos GP, Alexopoulos EC, Darviri C. A randomized controlled trial of the effects of a stress management programme during pregnancy. Complementary Therapies in Medicine. 2014; 22(2):203-11. [DOI:10.1016/j.ctim.2014.01.006] [PMID]
- Schaffer L, Jallo N, Howland L, James K, Glaser D, Arnell K. Guided imagery: An innovative approach to improving maternal sleep quality. The Journal of Perinatal & Neonatal Nursing. 2013; 27(2):151-9. [DOI:10.1097/JPN.0b013e3182870426] [PMID]
- Schlegel ML, Whalen JL, Williamsen PM. Integrative therapies for women with a high risk pregnancy during antepartum hospitalization. MCN. The American Journal of Maternal Child Nursing. 2016; 41(6):356-62. [DOI:10.1097/NMC.0000000000000279] [PMID]
- Wang W, Zhang Q, Qu F. The potential benefits of Chinese integrative medicine for pregnancy women during the COVID-19 pandemic. Integrative Medicine Research. 2020; 9(3):100461. [DOI:10.1016/j.imr.2020.100461] [PMID] [PMCID]
- Fathizade M, Abedini S, Mohseni SH. [The effect of pregnancy preparation classes on anxiety of mothers referring to Hormozgan Health Centers, Sirik (Persian)]. Preventive Care in Nursing & Midwifery Journal. 2016; 6(3):24-33. [Link]
- Rafiee B, Akbarzadeh M, Asadi N, Zare N. [Comparing the effects of educating of attachment and relaxation on anxiety in third trimester of pregnancy and postpartum depression in the primipara women (Persian)]. Journal of Hayat. 2013; 19(1):76-88. [Link]
- Gómez-Sánchez L, García-Banda G, Servera M, Verd S, Filgueira A, Cardo E. [Beneficios del mindfulness en mujeres embarazadas (Spanish)]. Medicina. 2020; 80(S 2):47-52. [PMID].
- Hulsbosch LP, Nyklíček I, Potharst ES, Meems M, Boekhorst MGBM, Pop VJM. Online mindfulness-based intervention for women with pregnancy distress: Design of a randomized controlled trial. BMC Pregnancy and Childbirth. 2020; 20(1):159. [DOI:10.1186/s12884-020-2843-0] [PMID] [PMCID]
- Spijkerman MP, Pots WT, Bohlmeijer ET. Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psychology Review. 2016; 45:102-14. [DOI:10.1016/j.cpr.2016.03.009] [PMID]
- Müller M, Matthies LM, Goetz M, Abele H, Brucker SY, Bauer A, et al. Effectiveness and cost-effectiveness of an electronic mindfulness-based intervention (eMBI) on maternal mental health during pregnancy: The mindmom study protocol for a randomized controlled clinical trial. Trials. 2020; 21(1):933. [DOI:10.1186/s13063-020-04873-3] [PMID] [PMCID]
- Tomfohr-Madsen LM, Campbell TS, Giesbrecht GF, Letourneau NL, Carlson LE, Madsen JW, et al. Mindfulness-based cognitive therapy for psychological distress in pregnancy: Study protocol for a randomized controlled trial. Trials. 2016; 17(1):498. [DOI:10.1186/s13063-016-1601-0] [PMID] [PMCID]
- Warriner S, Crane C, Dymond M, Krusche A. An evaluation of mindfulness-based childbirth and parenting courses for pregnant women and prospective fathers/partners within the UK NHS (MBCP-4-NHS). Midwifery. 2018; 64:1-10. [DOI:10.1016/j.midw.2018.05.004] [PMID]
- Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: Results of a pilot study. Archives of Women's Mental Health. 2008; 11(1):67-74. [DOI:10.1007/s00737-008-0214-3] [PMID]
- Perez-Blasco J, Viguer P, Rodrigo MF. Effects of a mindfulness-based intervention on psychological distress, well-being, and maternal self-efficacy in breast-feeding mothers: results of a pilot study. Archives of Women's Mental Health. 2013; 16(3):227-36. [DOI:10.1007/s00737-013-0337-z] [PMID]
- Woolhouse H, Mercuri K, Judd F, Brown SJ. Antenatal mindfulness intervention to reduce depression, anxiety and stress: A pilot randomised controlled trial of the MindBabyBody program in an Australian tertiary maternity hospital. BMC Pregnancy and Childbirth. 2014; 14:369. [DOI:10.1186/s12884-014-0369-z] [PMID] [PMCID]
- Beattie J, Hall H, Biro MA, East C, Lau R. Effects of mindfulness on maternal stress, depressive symptoms and awareness of present moment experience: A pilot randomised trial. Midwifery. 2017; 50:174-83. [DOI:10.1016/j.midw.2017.04.006] [PMID]
- Goetz M, Schiele C, Müller M, Matthies LM, Deutsch TM, Spano C, et al. Effects of a brief electronic mindfulness-based intervention on relieving prenatal depression and anxiety in hospitalized high-risk pregnant women: Exploratory pilot study. Journal of Medical Internet Research. 2020; 22(8):e17593. [DOI:10.2196/17593] [PMID] [PMCID]
- Lucena L, Frange C, Pinto ACA, Andersen ML, Tufik S, Hachul H. Mindfulness interventions during pregnancy: A narrative review. Journal of Integrative Medicine. 2020; 18(6):470-7. [DOI:10.1016/j.joim.2020.07.007] [PMID]
- Heydarpour S, Feli R, Yazdanbakhsh K, Heydarpour F. [The impact of mindfulness-based counseling on the levels of anxiety during pregnancy and on newborns’ physiological parameters (Persian)]. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2020; 6(1):106-17. [Link]
- Shahoie R, Karimi A, Sharifish S, Soufizadeh N, Khanpour F. [Evaluation of the effectiveness of mindfulness-based stress reduction on anxiety in pregnant women (Persian)]. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2019: 5(3):83-94. [Link]
- Kazemi Zahrani H, Behnampour N. [The effect of mindfulness-based stress reduction on the somatic, cognitive, behavioral anxiety and quality of sleep of pregnant mothers (Persian)]. Journal of Research in Behavioural Sciences. 2020; 18(2):227-36. [DOI:10.52547/rbs.18.2.227]
- Aslami E, Alipour A, Aghayusefi A, Najib F. [Assessing the effectiveness of mindfulness-based Islamic-spiritual schemas on anxiety of mothers pregnancy and infants physiological health (Persian)]. Health Psychology. 2015; 4(14):129-40. [Link]
- Nosratabadi M. The role of Islam in the health of pregnant women. Journal of Pizhūhish dar Dīn va Salāmat. 2021; 7(3):140-56. [DOI:10.22037/jrrh.v7i3.29008.]
- Niaz Azari M, Abdollahi M, Zabihi Hesari N K, Ashoori J. [Effect of spiritual group therapy on anxiety and quality of life among gestational diabetic females (Persian)]. Journal of Religion and Health. 2017; 5(1):11-20. [Link]
- Bodaghi E, Alipour F, Bodaghi M, Nori R, Peiman N, Saeidpour S. [The role of spirituality and social support in pregnant women’s anxiety, depression and stress symptoms (Persian)]. Journal of Community Health. 1396; 10(2):72-82. [Link]
- Azizi S, Pelarak F, Mohagheghi J. [Effectiveness of religious teachings in reducing anxiety in pregnant women (Persian)]. Journal of Religion and Health. 2017; 4(2):46-55. [Link]
- Khodakarami B, Soltani F, Golalizadeh G, Soltanian A, Mohagheghi H. [The effect of spiritual counseling on depression, anxiety and stress of pregnant women: A randomized clinical trial (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2015; 23(4):39-53. [Link]
- Irani M, Ghazanfarpour M, Nosrati Hadi Abad SF, Ramazanian Bafghi Z, Ahmadi A, Ashrafinia F. [Effect of listening to Qur’an recitation on severity of pain and anxiety during labor: A systematic review and mehta-analysis (Persian)]. Journal of Mazandaran University of Medical Sciences. 2020; 30(191):144-54. [Link]
- Naderyanfar F, Soleimani M, Shekhi H. [Effect of the voice of holy Quran on the anxiety of labor candidate pregnant women (Persian)]. Quran and Medicine. 2018; 4(1):1-4. [Link]
- Abbasi Z, Khodabande F, Darbaghi Moghadam, Taherpour M. [The effect of reading translations of Holy Quran on maternal anxiety (Persian]. Paper presented at: National Conference Quran Scholars and Medicine. 1 December 2013; Zanjan, Iran. [Link]
- Sahmeddini M, Zamani Lari M, Rahimian M, Danaei , Beigi N, Habibi H. [The effect of listening to the Quran on serum cortisol levels and anxiety in primiparous women during the first stage of labor (Persian)]. Iranian Journal of Obstetrics, Gynecology and Infertility. 2014; 17(99):1-7. [doi:10.22038 / ijogi.2014.2853]
- Kadkhodaei F, Mansouri A, Hajar S, Abak F, Pour BK, Nehbandani S. A comparative study on the effect of the voice of the holy Quran and Arendeshine music on the anxiety of the primiparous women of the natural provisional candidate. Asian Journal of Pharmaceutical Research and Development. 2019; 7(3):31-5. [DOI:10.22270/ajprd.v7i3.510]
- Yuni Fitri Hamidiyanti B, Gumilang Pratiwi I. Effect of listening to the Quran on anxiety level in primipara. Health, Spirituality and Medical Ethics. 2019; 6(1):52-6. [doi:10.29252/jhsme.6.1.52]
- Suhita BM, Mufidah A. Decrease of anxiety and pain delivery of mother inpartu primipara on first phase active by giving of murottal al Quran Arrahman in midwifery private clinic endang sumaningdyah city of Kediri. The 2nd Joint International Conferences, 2018 Sep 19. 2018; 2(2). [Link]
- Mir Bagher AjorPaz N, Ranjbar N. [Effects of recitation of holy quran on anxiety of women before cesarean section: A randomize clinical trial (Persian)]. Qom University of Medical Sciences Journal. 2010; 4(1):15-9. [Link]
- Namazi M, Amiraliakbari S, Mojab F, Talebi A, Alavi Majd H, jannesari S. Investigating the effect of citrus aurantium aroma on severity of labor pain during active phase of labor. Complementary Medicine Journal. 2014; 4(1):733-44. [Link]
- Ozgoli G, Torkashvand SH, Salehi Moghaddam, Borumandnia N, Mojab F, Minooee S. Comparison of Peppermint and Clove essential oil aroma on pain intensity and anxiety at first stage of labor (Persian)]. Iranian Journal of Obstetrics, Gynecology and Infertility. 2016; 19(21):1-11. [doi:10.22038/ijogi.2016.7665]
- Mirzae F, Keshtgar S, Kaviyani M, Rajaeifar A. [Changes in plasma concentrations of cortisol and serotonin and decreased levels of postpartum anxiety in nulliparous women following the smell of lavender essential oil (Persian)]. Journal of Kerman University of Medical Sciences. 2009; 16(3):245-54. [Link]
- Tafazoli M, Zaremobini F, Mokhber N, Emami A. [Citrus aurantium blossom and preoperative anxiety (Persian)]. Journal of Fundamentals Mental Health. 2011; 12(4):720-4
- Kheirkhah M, Setayesh Valipour N, Neisani Samani L, Haghani H. [Effect of aromatherapy with essential damask rose oil on anxiety of the active phase of labor nulliparous women (Persian)]. Nursing and Midwifery Journal. 2013; 11(6):428-33. [Link]
- Sharifipour F, Bakhteh A, Salary N. [The effect of Salvia aroma on la bor anxiety among primigravida and multigravida women: A randomized clinical trial (Persian)]. Journal of Hayat. 2017; 23(2):162-72. [Link]
- Ozgoli G, Aryamanesh Z, Mojab F, Alavi Majd H. [A study of inhalation of peppermint aroma on the pain and anxiety of the first stage of labor in nulliparous women: A randomized clinical trial (Persian)]. Qom University of Medical Sciences Journal. 2013; 7(3):21-7. [Link]
- Esmaelzadeh Saeieh S, Torkashvand Sh, Rahimzadeh Kivi M, Lotfi R, Akbari Kamrani M, Khosravi N. [Effect of aromatherapy with Boswellia Carteri on anxiety in first stage of labor in nulliparous women (Persian)]. Complementary Medicine Journal. 2015; 4(17):1314-23. [Link]
- Hamdamian S, Nazarpour S, Simbar M, Hajian S, Mojab F, Talebi A. Effects of aromatherapy with Rosa damascena on nulliparous women’s pain and anxiety of labor during first stage of labor. Journal of Integrative Medicine. 2018; 16(2):120-5. [DOI:10.1016/j.joim.2018.02.005] [PMID]
- Rashidi Fakari F, Tabatabaeichehr M, Kamali H, Rashidi Fakari F, Naseri M. Effect of inhalation of aroma of geranium essence on anxiety and physiological parameters during first stage of labor in nulliparous women: A randomized clinical trial. Journal of Caring Sciences. 2015; 4(2):135-41. [DOI:10.15171/jcs.2015.014] [PMID] [PMCID]
- Rashidi-Fakari F, Tabatabaeichehr M, Mortazavi H. The effect of aromatherapy by essential oil of orange on anxiety during labor: A randomized clinical trial. Iranian Journal of Nursing and Midwifery Research. 2015; 20(6):661-4. [DOI:10.4103/1735-9066.170001] [PMID] [PMCID]
- Moghadasi M, Soltanahmadi Z, Azizzadeh Forozi M, Mahdizadeh A, Jahani Y. [The effect of supportive counseling on reducing the anxiety of women at risk of preterm birth (Persian)]. Nursing and Midwifery Journal. 2016; 14(2):151-8. [Link]
- Andaroon N, Kordi M, Kimiaee A, Esmaily H. [Effect of individual counseling program by a midwife on anxiety during pregnancy in nulliparous women (Persian)]. Iranian Journal of Obstetrics, Gynecology and Infertility. 2017; 20(12):86-95. [doi:10.22038 / ijogi.2017.10434]
- Barjasteh A, Alizade S, Moghaddam Tabrizi F. [Antenatal anxiety and pregnancy worries in association with marital and social support (Persian)]. Nursing and Midwifery Journal. 2016; 14(6):504-15. [Link]
- Mohammadpour M, Mohammad-Alizadeh Charandabi S, Malakouti J, Mohammadi MN, Mirghafourvand M. The effect of counseling on fathers’ stress and anxiety during pregnancy: A randomized controlled clinical trial. BMC Psychiatry. 2021; 21(1):208. [DOI:10.1186/s12888-021-03217-y] [PMID] [PMCID]
- Imanparast R, Bermas H, Danesh S, Ajoudani Z. [The effect of cognitive behavior therapy on anxiety reduction of first normal vaginal delivery (Persian)]. Journal of Shahid Sadoughi University of Medical Sciences. 2014; 22(1):974-980. [Link]
- Matvienko-Sikar K, Dockray S. Effects of a novel positive psychological intervention on prenatal stress and well-being: A pilot randomised controlled trial. Women and Birth. 2017; 30(2):e111-8. [DOI:10.1016/j.wombi.2016.10.003] [PMID]
- Ghorbani S, Jourabchi Z, Sarichloo ME, Olfati F. [The effect of group counseling based on cognitive behavioral therapy on anxiety of pregnant women with constipation: Clinical trial (Persian)]. Avicenna Journal of Nursing and Midwifery Care. 2020; 28(4):32-44. [DOI:10.30699/ajnmc.28.4.32]
- Bright KS, Mughal MK, Wajid A, Lane-Smith M, Murray L, Roy N, et al. Internet-based interpersonal psychotherapy for stress, anxiety, and depression in prenatal women: Study protocol for a pilot randomized controlled trial. Trials. 2019; 20(1):814. [DOI:10.1186/s13063-019-3897-z] [PMID] [PMCID]
- Toker E, Kömürcü N. Effect of Turkish classical music on prenatal anxiety and satisfaction: A randomized controlled trial in pregnant women with pre-eclampsia. Complementary Therapies in Medicine. 2017; 30:1-9. [DOI:10.1016/j.ctim.2016.11.005] [PMID]
- Garcia-Gonzalez J, Ventura-Miranda MI, Requena-Mullor M, Parron-Carreño T, Alarcon-Rodriguez R. State-trait anxiety levels during pregnancy and foetal parameters following intervention with music therapy. Journal of Affective Disorders. 2018; 232:17-22. [DOI:10.1016/j.jad.2018.02.008] [PMID]
- Arranz Betegón Á, García M, Parés S, Montenegro G, Feixas G, Padilla N, et al. A program aimed at reducing anxiety in pregnant women diagnosed with a small-for-gestational-age fetus: Evaluative findings from a Spanish study. The Journal of Perinatal & Neonatal Nursing. 2017; 31(3):225-35. [DOI:10.1097/JPN.0000000000000270] [PMID]
- Corbijn van Willenswaard K, Lynn F, McNeill J, McQueen K, Dennis CL, Lobel M, et al. Music interventions to reduce stress and anxiety in pregnancy: A systematic review and meta-analysis. BMC Psychiatry. 2017; 17(1):271. [DOI:10.1186/s12888-017-1432-x] [PMID] [PMCID]
- Nanbakhsh F, Zadeh Mohammadi A, Jalili N, Ahmadnejad E. [The effect of music in reducing the pain and stress during delivery (Persian)]. Studies in Medical Sciences. 2009; 20(3):209-14. [Link]
- Hoseini Nasab D, Taghavi S, Ahmadiyan S. [The effect of pregnancy training on anxiety, pain and duration of labor pains in mothers (Persian)]. Medical Journal of Tabriz University of Medical Sciences. 2009; 31(4):24-30. [Link]
- Bogaerts AF, Devlieger R, Nuyts E, Witters I, Gyselaers W, Van den Bergh BR. Effects of lifestyle intervention in obese pregnant women on gestational weight gain and mental health: A randomized controlled trial. International Journal of Obesity. 2013; 37(6):814-21. [DOI:10.1038/ijo.2012.162] [PMID]
- Urizar GG Jr, Muñoz RF. Impact of a prenatal cognitive-behavioral stress management intervention on salivary cortisol levels in low-income mothers and their infants. Psychoneuroendocrinology. 2011; 36(10):1480-94. [DOI:10.1016/j.psyneuen.2011.04.002] [PMID] [PMCID]
- Urizar GG Jr, Yim IS, Rodriguez A, Schetter CD. The SMART moms program: A randomized trial of the impact of stress management on perceived stress and cortisol in low-income pregnant women. Psychoneuroendocrinology. 2019; 104:174-84. [DOI:10.1016/j.psyneuen.2019.02.022] [PMID]
- Golshani F, Gholmohammad Nejad GH, Aghdasi A. [The effectiveness of teaching life skills during pregnancy on pregnant mothers’ mental health (Persian)]. Scientific Journal of Education and Evaluation (Quarterly), 2014; 7(26):89-101. [Link]
- Newham JJ, Westwood M, Aplin JD, Wittkowski A. State-trait anxiety inventory (STAI) scores during pregnancy following intervention with complementary therapies. Journal of Affective Disorders. 2012; 142(1-3):22-30. [DOI:10.1016/j.jad.2012.04.027] [PMID]
- javanbakht M, Hejazi Kenari R, Ghasemi M. Effects of yoga on depression and anxiety of women. Complementary Therapies in Clinical Practice. 2009; 15(2):102-4. [DOI:10.1016/j.ctcp.2009.01.003] [PMID]
- Satyapriya M, Nagarathna R, Padmalatha V, Nagendra HR. Effect of integrated yoga on anxiety, depression & well being in normal pregnancy. Complementary Therapies in Clinical Practice. 2013; 19(4):230-6. [DOI:10.1016/j.ctcp.2013.06.003] [PMID]
- Newham JJ, Wittkowski A, Hurley J, Aplin JD, Westwood M. Effects of antenatal yoga on maternal anxiety and depression: A randomized controlled trial. Depression and Anxiety. 2014; 31(8):631-40. [DOI:10.1002/da.22268] [PMID]
- van der Zwan JE, Huizink AC, Lehrer PM, Koot HM, de Vente W. The effect of heart rate variability biofeedback training on mental health of pregnant and non-pregnant women: A randomized controlled trial. International Journal of Environmental Research and Public Health. 2019; 16(6):1051. [DOI:10.3390/ijerph16061051] [PMID] [PMCID]
- Mirzaee F, Kaviani M, Jafari P. [Effect of reflexology on anxiety level in nuliparous women (Persian)]. Journal of Hayat. 2010; 16(1):65-71. [Link]
- Bazrafshan M, Ghorbani Z. [The effect of slow stroke back massages on anxiety among primigravid women (Persian)]. Journal of Hayat. 2010; 16(1):34-40. [Link]
- Castel S, Creveuil C, Beunard A, Blaizot X, Proia N, Guillois B. Effects of an intervention program on maternal and paternal parenting stress after preterm birth: A randomized trial. Early Human Development. 2016; 103:17-25. [DOI:10.1016/j.earlhumdev.2016.05.007] [PMID]
- Mirzakhani K, Hejazinia Z, Golmakani N, Mirteimouri M, Sardar MA, Shakeri MT. [The effect of execution of exercise program with birth ball during pregnancy on anxiety rate in nulliparous women (Persian)]. Iranian Journal of Obstetrics, Gynecology and Infertility. 2014; 17(117):8-16. [doi:10.22038/ijogi.2014.3474]
- Gholami A, Karimi F, Ghasempour Z, Abolhassani M, Rabiee N. [Comparison of the effect of kangaroo care and infant massage on the level of maternal anxiety and neonatal pain (Persian)]. Journal of Babol University of Medical Sciences. 2021; 23(1):90-7. [doi:10.22088/jbums.23.1.90]
- Simó S, Zúñiga L, Izquierdo MT, Rodrigo MF. Effects of ultrasound on anxiety and psychosocial adaptation to pregnancy. Archives of Women's Mental Health. 2019; 22(4):511-8. [DOI:10.1007/s00737-018-0918-y] [PMID]
- Barrio-Forné N, Gasch-Gallén Á. Companionship as a method to reduce anxiety in pregnant women hospitalized during their third trimester. Revista da Escola de Enfermagem da U S P. 2021; 55:e03749. [DOI:10.1590/s1980-220x2020018603749] [PMID]
- Makvandi S, Zargar Shoshtari S, Montazeri S, Ahangarpour A. [The effect of chewing sugar-free gum on the anxiety level of active phase of labor in nulliparous women (Persian)]. Razi Journal of Medical Sciences. 2013; 20(112):9-15. [Link]
- Ebrahimian A, Bilandi RR, Bilandī MR, Sabzeh Z. Comparison of the effectiveness of virtual reality and chewing mint gum on labor pain and anxiety: a randomized controlled trial. BMC Pregnancy and Childbirth. 2022; 22(1):49. [DOI:10.1186/s12884-021-04359-3] [PMID] [PMCID]
- Rahimi F, Moeni Mehr M. [Effect of different relaxation methods on pregnancy and childbirth: A systematic review (Persian)]. Journal of Shahid Sadoughi University of Medical Sciences. 2021; 29(2):3462-78. [DOI:10.18502/ssu.v29i2.6085]
Type of Study: Review |
Subject:
Obstetrics and Gynecology
Received: 2022/03/7 | Accepted: 2022/06/22 | Published: 2022/07/1
Received: 2022/03/7 | Accepted: 2022/06/22 | Published: 2022/07/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |