

Volume 28, Issue 4 (Autumn 2022)
Intern Med Today 2022, 28(4): 514-529 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aghili S M, Farhang A. Investigating the Effectiveness of Dialectical Behavior Therapy on Resilience, Psychological Flexibility, and Glycemic Control of Diabetic Patients. Intern Med Today 2022; 28 (4) :514-529
URL: http://imtj.gmu.ac.ir/article-1-3940-en.html
URL: http://imtj.gmu.ac.ir/article-1-3940-en.html
1- Department of Psychology, Payam Noor University, Tehran, Iran. , dr_aghili1398@yahoo.com
2- Department of Psychology, Faculty of Humanities, Payam Noor University, Gorgan, Iran.
2- Department of Psychology, Faculty of Humanities, Payam Noor University, Gorgan, Iran.
Full-Text [PDF 4931 kb]
(904 Downloads)
| Abstract (HTML) (1542 Views)
Full-Text: (1360 Views)
Introduction
Diabetes is a growing chronic disease that, in addition to affecting the individual’s clinical condition, imposes high costs on societies worldwide [1]. This chronic disease can be declared a hidden pandemic according to the statistics and its increasing trend in the world. The global prevalence of diabetes was about 371 million people in 2012, which is estimated to reach about 552 million people by 2030 [2]. Although the statistics regarding the prevalence of diabetes in Iran are different, the Endocrine and Metabolism Research Center of Shahid Beheshti University of Medical Sciences, Tehran University of Medical Sciences, and Kermanshah University of Medical Sciences, reported the prevalence of diabetes from 2% to 10% to more than 12% and 7%, respectively [3]. Diabetes is a complex metabolic disorder, characterized by fasting blood sugar levels greater than 126 mg/dL, random sugar greater than 200 mg/dL with symptoms of binge drinking and hyperuria, and 2-h postprandial blood sugar greater than 200 mg/dL. A deciliter or sugar 2 h after consuming 75 grams of glucose is determined to be more than 200 mg/dL [4]. Hyperglycemia occurs as a result of impaired secretion or function of insulin [5]. There are two main types of diabetes. In subjects with type 1 diabetes, little or no insulin is produced, while individuals with type 2 diabetes cannot use insulin [6]. Type 2 diabetes is a chronic multifactorial disorder that is associated with organ damage and long-term hyperglycemia. The complications of diabetes are related to the lack of glycemic control in patients with type 2 diabetes, which leads to increased mortality in these patients [7].
Since patients face many challenges, such as the pressures caused by the control and treatment of the disease, the cost, the need for frequent visits to the doctor, worry about the future of the disease, and the possibility of having children, diabetes, similar to other chronic diseases, leads to stress and reduced resilience patients [8]. Resilience is a psychological and personality trait that plays an important role in stressful experiences and stressful events [9]. Resilience is the ability to withstand stress and regain balance after experiencing stressful situations [10], and it helps people to have high willpower and motivation [11]. Considering that resilience is both innate and acquired, people can increase their resilience by learning related skills. In other words, resilience can encourage hope in clinical experiences, and the ability to return to the initial state after difficulty with those factors can lead to adaptive outcomes even in challenging and threatening conditions [12].
The results of studies show that high levels of resilience help diabetic patients to use positive emotions to overcome adverse experiences and return to a favorable situation by increasing the levels of positive emotions while strengthening their dignity [13]. Studies showed that psychological flexibility predicts anxiety and stress in patients with diabetes [14].
Psychological flexibility is a set of behaviors that people perform in line with their determined values [15]. According to Wang, Zhou, Yu, and Ron, psychological flexibility refers to the ability to communicate with the present and that a person can change their behavior based on what is expected of them in a particular situation or persist in their current behavior [16]. Accordingly, it can be said that the absence of behaviors that align with the individual’s values makes the individual feel that their life is meaningless, purposeless, and full of emotional pain [17]. This leads to a decrease in the psychological flexibility of individuals [18]. Psychological flexibility has such a capability that by changing people’s thoughts and behavior, individuals can produce adaptive responses to environmental changes [19]. It is achieved through 6 processes: Reception, neutralization (disruption), context self, making contact with the current moment, values, and committed action [20].
Nowadays, various treatment approaches are applied to patients with diabetes. One of the new treatments of the third wave that is currently being used for a wide range of chronic diseases, including diabetes, is dialectical behavior therapy [21]. Dialectical behavior therapy as a worldview or philosophical perspective guides clinical professionals in the direction of making theoretical hypotheses appropriate to clients’ problems and their treatment [22]. The goal of dialectical behavior therapy is to create a balance between change and acceptance so that clients can regulate their emotional responses to events [23].
In this method, skill training, including training in effective interpersonal skills, mindfulness, emotional regulation, increasing failure tolerance, reception, and validation of emotions is emphasized [24]. Dialectical behavior therapy is a set of techniques to make changes in how a person thinks and behaves, reduce negative thoughts, change the lifestyle, and also achieve behavioral and emotional stability [25]. Dialectical behavior therapy is effective in reducing the stress of diabetic patients [26 ]. In this regard, the results of the study by Khakshur et al. showed that the dialectical behavior therapy method has significantly increased cognitive flexibility and reduced stress in patients with type 2 diabetes [21].
Bahrami and Zahedi found that dialectical behavior therapy could significantly increase the life expectancy and resilience of women [27]. Ramaiya et al. showed that dialectical behavior therapy can be effective in improving women’s resilience [28]. The study by Lee and Mason showed that short-term dialectical behavior therapy is effective in the psychological resilience of a group of clients in counseling centers [30].
The effect of previous treatments, including third-wave treatments, in improving mental health and reducing blood sugar in diabetic patients has been confirmed. However, this treatment has some limitations, such as the failure to improve many patients, the existence of numerous guidelines and treatment instructions for each disorder, the lack of cost-effectiveness in terms of time and cost for specialists and references, long-term and numerous internships for the treatment of each of the disorders, and the complexity of the process of publication and compilation of treatment instructions for the producers. In addition, in the study by Khakshur et al. [21], dialectical behavior therapy was only conducted on women with diabetes; therefore, considering the mentioned limitations, this research investigates the effectiveness of this treatment on both sexes along with other variables, such as resilience and the level of glycemic control.
The reason for using dialectical behavior therapy for patients with diabetes is the existence of low cognitive self-awareness and mindfulness among chronic patients, which causes a lack of sufficient awareness of mental processes. Accordingly, it seems that dialectical behavior therapy can open a new window for the psychological and emotional processes of these individuals, and the lack of research to investigate the effectiveness of dialectical behavior therapy on the mentioned variables in the present study in the statistical population of patients with diabetes encourages us to answer whether dialectical behavior therapy affects resilience, psychological flexibility, and the level of glycemic control in diabetic patients.
Materials and Methods
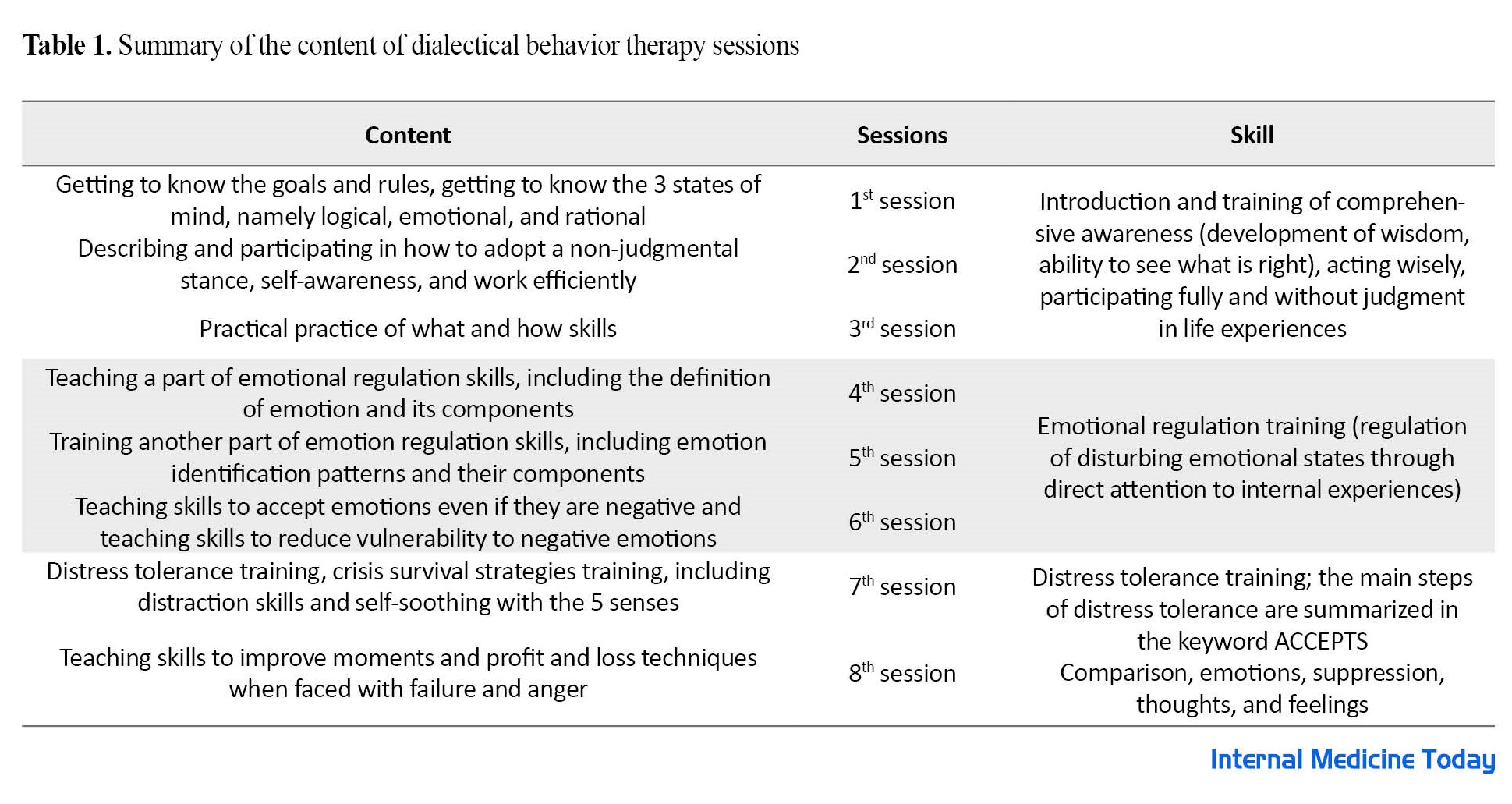
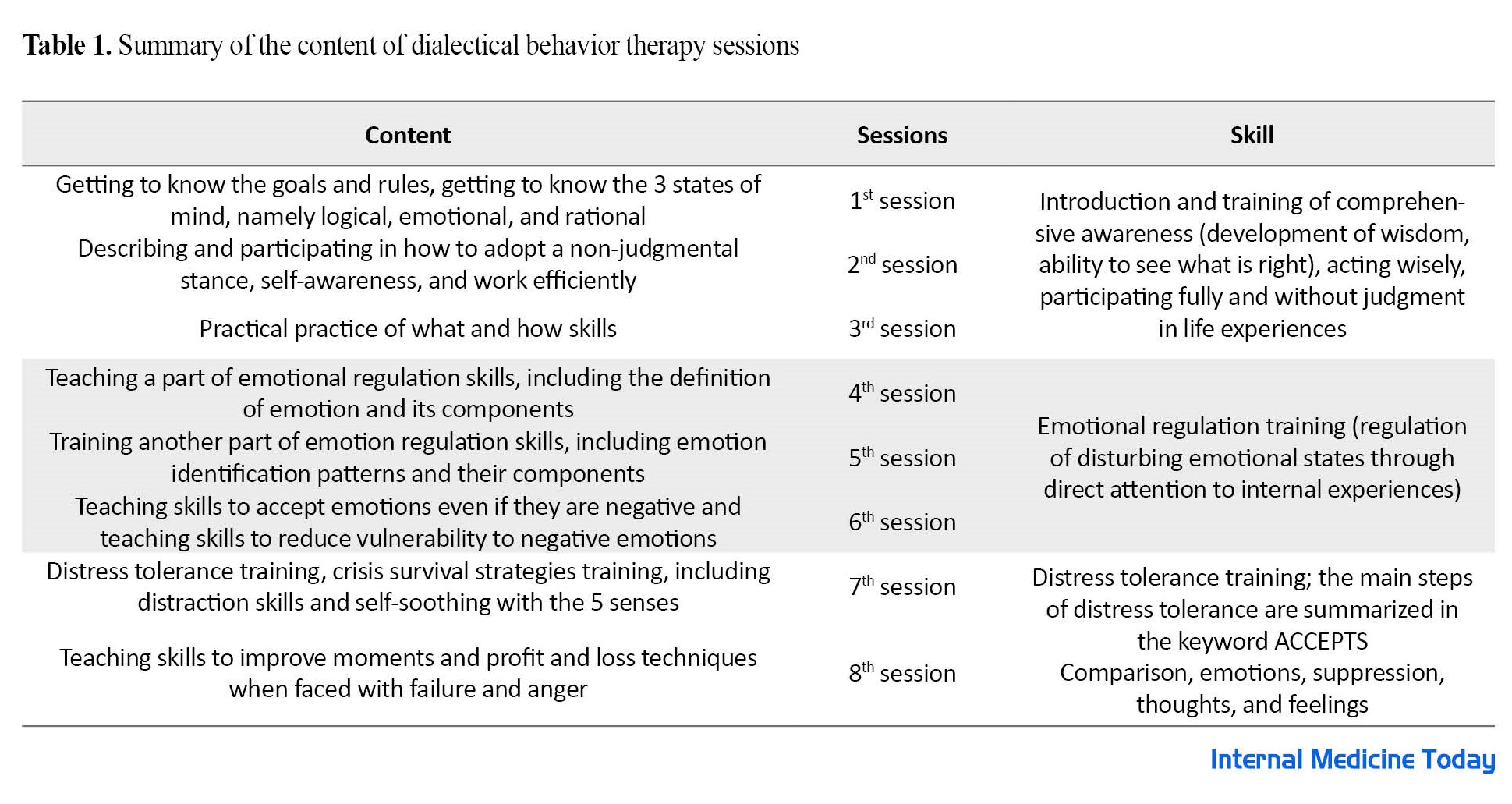
The present study had a semi-experimental design with a pre-test/post-test design and a control group. The statistical population included all people with diabetes who were referred to Sayad Hospital in Gorgan City, Iran in May 2022. From this statistical population, at the end of May, 30 patients were selected via available sampling and were randomly divided into an experimental (n=15) and a control group (n=15). In June 2022, the experimental and control groups participated in the pre-test. Then, the experimental group was trained in dialectical behavior therapy in eight 60-min sessions (Saturday and Tuesday every week) (Table 1), while the control group did not receive any psychological intervention during the research.
In July, a post-test was conducted on the experiment and control groups. The criteria for entering the study were not suffering from a severe psychiatric disease at the same time as having diabetes, the lack of amputation (limb amputation) and disability, not using psychiatric drugs, not experiencing diabetic coma, having at least a high school diploma, being over 18 years of age, glycosylated hemoglobin higher than 7, and not receiving any other educational program before and during the mindfulness intervention. The exclusion criteria were the absence of more than two sessions, non-cooperation, not performing the assignments specified in the class, and unwillingness to continue participating in the research process. To comply with ethical principles in the research, the control group was assured that they will receive the interventions after the completion of the research process. Also, before and after the treatment program, glycosylation levels were measured as an index to measure glycemic control. In this study, the covariance analysis was used to analyze the data. Meanwhile, the data were analyzed via the SPSS software, version 22.
Study instruments
Psychological resilience questionnaire
The Dennis and Vanderwall psychological resilience questionnaire was designed in 2010 [30]. This questionnaire included 20 questions to measure a type of psychological flexibility that is necessary for a person’s success to challenge and replace ineffective thoughts with more efficient ones and has 3 subscales of alternatives, control, and alternatives for human behavior. This questionnaire is based on a 7-point Likert scale ranging from 1 (completely disagree) to 7 (completely agree). The range of questionnaire scores is from 20 to 140. Higher scores indicate greater psychological flexibility. The cut-off score for this questionnaire is 70. In the research by Dennis and Vanderwaal, the concurrent validity of this questionnaire with the Beck depression questionnaire was - 0.39, and its convergent validity with the psychological flexibility scale of Martin and Robin was 0.75 [30]. Masuda and Tali also calculated the reliability of this questionnaire at 0.82 [31]. The reliability of this questionnaire in the Ali Akbari Dehkordi et al. study was obtained at 0.79 using the Cronbach α coefficient [18].
Connor and Davidson resilience questionnaire
Connor and Davidson designed the resilience questionnaire in 2003 to measure the level of resilience in different people [32]. This scale is self-reported and has 25 questions. The scoring of this scale is based on a Likert scale ranging from 0 (completely false) to 4 (always true). To obtain the total score of the questionnaire, the total scores of all the questions are added together. This score ranges from 0 to 100. Higher scores indicate greater resilience of the respondent. The cut-off point for this questionnaire is 50; that is, a score higher than 50 indicates people who have higher resilience, and higher scores demonstrate a higher level of resilience. The reliability (by re-test method and Cronbach α) and validity (by factor analysis, convergent, and divergent validity) have been verified in different groups (normal and at risk). Connor and Davidson reported the Cronbach α coefficient of the resilience scale at 0.89. Also, the reliability coefficient obtained from the re-test method in a 4-week interval was 0.87. Khoshnazari, Hosseini, Falahi Khoshkotab, and Bakhshi translated the resilience questionnaire and reported its content validity as 0.84 and its reliability coefficient as 0.94 [33]. In addition, the Cronbach α in the present study was 0.86.
Measurement of blood sugar factor: In this research, the fasting ELISA method was used to measure this factor in diabetic patients using a laboratory kit in the pre-test and post-test stages.
Results
The demographic findings showed that the mean age of the participants in the experimental group was 47.9 years while the control group was 49.3 years. Also, 46.2% of the participants had a diploma, 35.2% had a bachelor’s degree, and 18.6% had a postgraduate degree. Among the participants, 84.1% were married and 15.9% were single. The Mean±SD of the research variables are presented in Table 2.
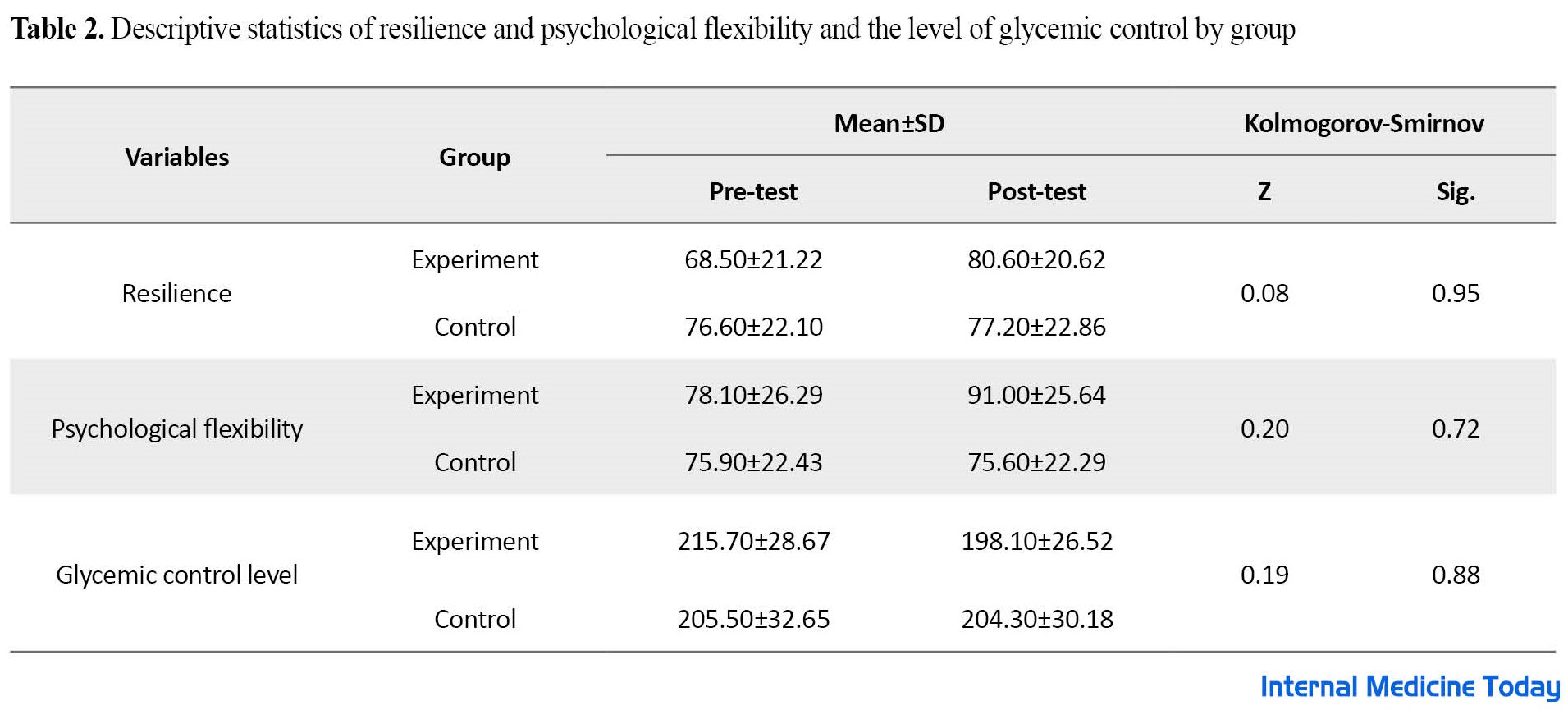
Table 2 shows the Mean±SD of the variables of resilience and psychological flexibility and the level of glycemic control in the pre-test and post-test phases. The results showed a significant difference in the scores of the experimental group after dialectical behavior therapy. Also, the Kolmogorov-Smirnov test shows that the assumption of normality is established for all variables of resilience, psychological flexibility, and the level of glycemic control (P<0.05). The results of the Lon test showed that the assumption of homogeneity of variance was also valid for all variables of resilience (F=0.262, P=0.615), psychological flexibility (F=1.45, P=0.243), and glycemic control (F=0.409, P=0.530). The results of multivariate covariance analysis are reported in Table 3
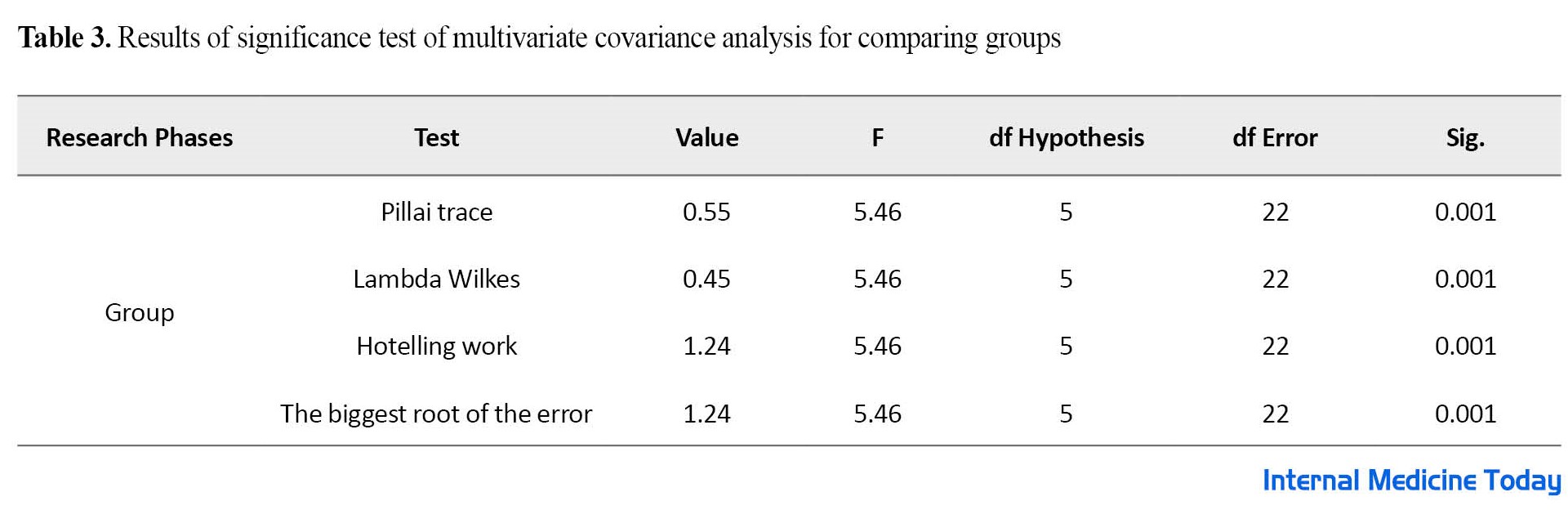
According to Table 3, the results of the multivariate covariance analysis indicate that the F obtained in all tests is significant at P<0.05 level with degrees of freedom at 5 and 22. The results showed a significant difference in the research variables after removing the pre-test effect, P<0.05 and (df=5 and df=22) and (F=5.46 and Pillai trace=0.55). In the following, univariate analysis of the covariance test was used for a more detailed understanding and investigation of the separate effect of the independent variable on the dependent variables.
The results of Table 4 show a significant difference between the two experimental and control groups in the variables of resilience, psychological flexibility, and the amount of glycemic control (P<0.001).
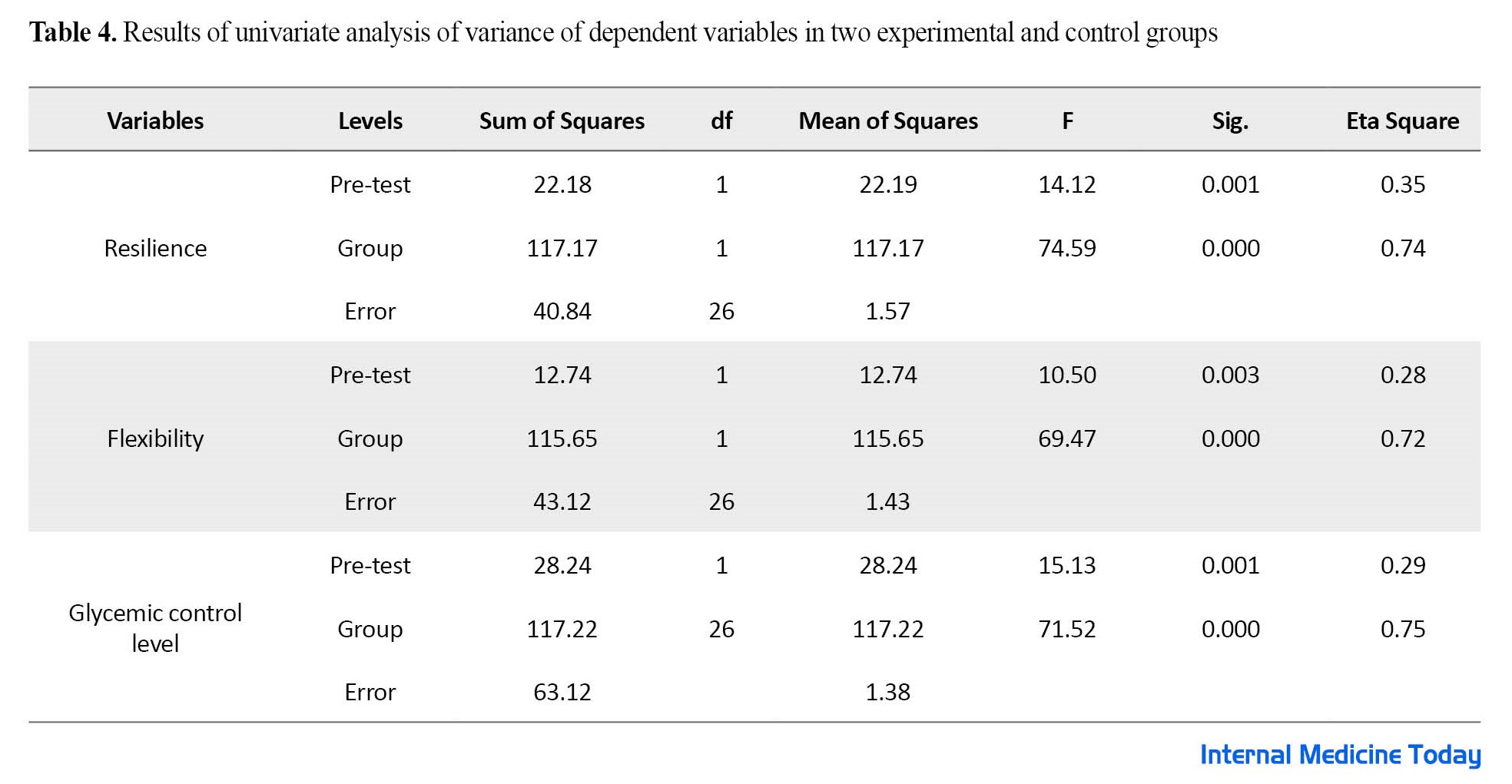
The obtained Eta coefficient indicates that the variance related to the difference between the two groups in the post-test is because of the effectiveness of dialectical behavior therapy.
Discussion
This research was conducted to investigate the effectiveness of dialectical behavior therapy on the resilience, flexibility, and glycemic control of diabetic patients. The findings showed that dialectical behavior therapy is effective in increasing resilience, flexibility, and glycemic control in patients. This finding is in line with the results of other studies [21, 25-29].
In explaining this finding, patients are taught various behavioral therapy skills concerning resilience to solve problems, social support, optimism, tolerance of chaos, purposefulness and hope, and having an enjoyable life. A dialectic that includes basic comprehensive awareness, distress tolerance, emotion regulation, and efficiency between individuals was taught and its practical practice was discussed in a group session. Dialectical therapy by using communication skills, self-awareness, problem-solving, behavior control, asking for help, optimism, eliminating misconceptions, empathy, and decision-making power can increase hopeful and purposeful thinking in patients, thereby improving mental health and helping improve resilience skills [27]. In a more specific way, due to the characteristics and chronic nature of diabetes, accepting the sufferings and bearing the disturbances caused by diabetes is very vital in the resilience of these people; therefore, teaching the skills of coping with disturbance has been effective in this group by improving the level of pain tolerance caused by living with diabetes and preventing it from turning into psychological suffering. On the other hand, since dialectical behavior therapy has placed mindfulness at the center of its work, it can be effective in promoting resilience by increasing the individual’s focus and teaching life in the present moment, and adopting a non-judgmental approach. Emotional regulation training has been effective in promoting resilience through reducing emotional vulnerability and learning methods to reduce negative vulnerability and increase emotional toughness [28].
The main core of dialectical behavior therapy is mindfulness and emotional regulation skills that teach patients to be aware of their emotions, thoughts, and behaviors, to face emotions, and to act against strong emotional desires (increasing cognitive flexibility). In addition, practicing non-fusion of thought and excitement is effective for regulating emotions and reducing instability and impulsivity [24]. Therefore, through dialectical behavior therapy and the techniques and skills a person becomes aware of the impact of the relationship between thoughts and emotions, and automatic maladaptive evaluation is identified, and this cognitive re-evaluation will increase flexibility in thinking. Doing mindfulness exercises by increasing an individual’s ability to turn their attention from what is not useful or effective (such as focusing on negative thoughts) to what is useful and effective can help to moderate their emotional experience [21], which makes people with diabetes have more cognitive flexibility, based on which they find alternatives to difficult situations, find difficult situations controllable, and find meaning and positive alternatives for other subject’s events and social behaviors [18]. Accordingly, dialectical behavior therapy can reduce psychological damage, such as anxiety and variables by creating the ability to tolerate disturbance and create more psychological peace. Also, dialectical behavior therapy as a supportive treatment that requires a strong relationship between the patient and the therapist can develop skills such as tolerance of helplessness, mindfulness, self-regulation of emotions, and efficient skills in patients by providing new strategies to moderate the effects of uncomfortable conditions and increasing psychological flexibility, it helps patients with diabetes to cope with the painful experiences of diabetes [15].
Conclusion
The results of the research showed that dialectical behavioral therapy skills, such as distress tolerance, emotion regulation, and interpersonal efficiency led to an increase in resilience and psychological flexibility in patients with diabetes. The present research was conducted on diabetic patients of Gorgan City, Iran. Therefore, if there is a change in the number and gender of the population and the statistical sample, different results may be obtained. It is suggested that this research be conducted as a case study in several statistical populations (cardiovascular patients, other cities, women, and men) and the results be compared with each other. It is suggested that policymakers in the field of health and treatment try to increase the resilience and flexibility of diabetic patients through various methods such as dialectical behavior therapy.
Ethical Considerations
Compliance with ethical guidelines
This project approved by received the the Research Vice-Chancellor of Payam-e-Noor University (Code: IR.PNU.REC.1401.024).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
The both authord contributed equally to the writing of the article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
All authors thank all the participants for their cooperation in this research.
References
Diabetes is a growing chronic disease that, in addition to affecting the individual’s clinical condition, imposes high costs on societies worldwide [1]. This chronic disease can be declared a hidden pandemic according to the statistics and its increasing trend in the world. The global prevalence of diabetes was about 371 million people in 2012, which is estimated to reach about 552 million people by 2030 [2]. Although the statistics regarding the prevalence of diabetes in Iran are different, the Endocrine and Metabolism Research Center of Shahid Beheshti University of Medical Sciences, Tehran University of Medical Sciences, and Kermanshah University of Medical Sciences, reported the prevalence of diabetes from 2% to 10% to more than 12% and 7%, respectively [3]. Diabetes is a complex metabolic disorder, characterized by fasting blood sugar levels greater than 126 mg/dL, random sugar greater than 200 mg/dL with symptoms of binge drinking and hyperuria, and 2-h postprandial blood sugar greater than 200 mg/dL. A deciliter or sugar 2 h after consuming 75 grams of glucose is determined to be more than 200 mg/dL [4]. Hyperglycemia occurs as a result of impaired secretion or function of insulin [5]. There are two main types of diabetes. In subjects with type 1 diabetes, little or no insulin is produced, while individuals with type 2 diabetes cannot use insulin [6]. Type 2 diabetes is a chronic multifactorial disorder that is associated with organ damage and long-term hyperglycemia. The complications of diabetes are related to the lack of glycemic control in patients with type 2 diabetes, which leads to increased mortality in these patients [7].
Since patients face many challenges, such as the pressures caused by the control and treatment of the disease, the cost, the need for frequent visits to the doctor, worry about the future of the disease, and the possibility of having children, diabetes, similar to other chronic diseases, leads to stress and reduced resilience patients [8]. Resilience is a psychological and personality trait that plays an important role in stressful experiences and stressful events [9]. Resilience is the ability to withstand stress and regain balance after experiencing stressful situations [10], and it helps people to have high willpower and motivation [11]. Considering that resilience is both innate and acquired, people can increase their resilience by learning related skills. In other words, resilience can encourage hope in clinical experiences, and the ability to return to the initial state after difficulty with those factors can lead to adaptive outcomes even in challenging and threatening conditions [12].
The results of studies show that high levels of resilience help diabetic patients to use positive emotions to overcome adverse experiences and return to a favorable situation by increasing the levels of positive emotions while strengthening their dignity [13]. Studies showed that psychological flexibility predicts anxiety and stress in patients with diabetes [14].
Psychological flexibility is a set of behaviors that people perform in line with their determined values [15]. According to Wang, Zhou, Yu, and Ron, psychological flexibility refers to the ability to communicate with the present and that a person can change their behavior based on what is expected of them in a particular situation or persist in their current behavior [16]. Accordingly, it can be said that the absence of behaviors that align with the individual’s values makes the individual feel that their life is meaningless, purposeless, and full of emotional pain [17]. This leads to a decrease in the psychological flexibility of individuals [18]. Psychological flexibility has such a capability that by changing people’s thoughts and behavior, individuals can produce adaptive responses to environmental changes [19]. It is achieved through 6 processes: Reception, neutralization (disruption), context self, making contact with the current moment, values, and committed action [20].
Nowadays, various treatment approaches are applied to patients with diabetes. One of the new treatments of the third wave that is currently being used for a wide range of chronic diseases, including diabetes, is dialectical behavior therapy [21]. Dialectical behavior therapy as a worldview or philosophical perspective guides clinical professionals in the direction of making theoretical hypotheses appropriate to clients’ problems and their treatment [22]. The goal of dialectical behavior therapy is to create a balance between change and acceptance so that clients can regulate their emotional responses to events [23].
In this method, skill training, including training in effective interpersonal skills, mindfulness, emotional regulation, increasing failure tolerance, reception, and validation of emotions is emphasized [24]. Dialectical behavior therapy is a set of techniques to make changes in how a person thinks and behaves, reduce negative thoughts, change the lifestyle, and also achieve behavioral and emotional stability [25]. Dialectical behavior therapy is effective in reducing the stress of diabetic patients [26 ]. In this regard, the results of the study by Khakshur et al. showed that the dialectical behavior therapy method has significantly increased cognitive flexibility and reduced stress in patients with type 2 diabetes [21].
Bahrami and Zahedi found that dialectical behavior therapy could significantly increase the life expectancy and resilience of women [27]. Ramaiya et al. showed that dialectical behavior therapy can be effective in improving women’s resilience [28]. The study by Lee and Mason showed that short-term dialectical behavior therapy is effective in the psychological resilience of a group of clients in counseling centers [30].
The effect of previous treatments, including third-wave treatments, in improving mental health and reducing blood sugar in diabetic patients has been confirmed. However, this treatment has some limitations, such as the failure to improve many patients, the existence of numerous guidelines and treatment instructions for each disorder, the lack of cost-effectiveness in terms of time and cost for specialists and references, long-term and numerous internships for the treatment of each of the disorders, and the complexity of the process of publication and compilation of treatment instructions for the producers. In addition, in the study by Khakshur et al. [21], dialectical behavior therapy was only conducted on women with diabetes; therefore, considering the mentioned limitations, this research investigates the effectiveness of this treatment on both sexes along with other variables, such as resilience and the level of glycemic control.
The reason for using dialectical behavior therapy for patients with diabetes is the existence of low cognitive self-awareness and mindfulness among chronic patients, which causes a lack of sufficient awareness of mental processes. Accordingly, it seems that dialectical behavior therapy can open a new window for the psychological and emotional processes of these individuals, and the lack of research to investigate the effectiveness of dialectical behavior therapy on the mentioned variables in the present study in the statistical population of patients with diabetes encourages us to answer whether dialectical behavior therapy affects resilience, psychological flexibility, and the level of glycemic control in diabetic patients.
Materials and Methods
The present study had a semi-experimental design with a pre-test/post-test design and a control group. The statistical population included all people with diabetes who were referred to Sayad Hospital in Gorgan City, Iran in May 2022. From this statistical population, at the end of May, 30 patients were selected via available sampling and were randomly divided into an experimental (n=15) and a control group (n=15). In June 2022, the experimental and control groups participated in the pre-test. Then, the experimental group was trained in dialectical behavior therapy in eight 60-min sessions (Saturday and Tuesday every week) (Table 1), while the control group did not receive any psychological intervention during the research.
In July, a post-test was conducted on the experiment and control groups. The criteria for entering the study were not suffering from a severe psychiatric disease at the same time as having diabetes, the lack of amputation (limb amputation) and disability, not using psychiatric drugs, not experiencing diabetic coma, having at least a high school diploma, being over 18 years of age, glycosylated hemoglobin higher than 7, and not receiving any other educational program before and during the mindfulness intervention. The exclusion criteria were the absence of more than two sessions, non-cooperation, not performing the assignments specified in the class, and unwillingness to continue participating in the research process. To comply with ethical principles in the research, the control group was assured that they will receive the interventions after the completion of the research process. Also, before and after the treatment program, glycosylation levels were measured as an index to measure glycemic control. In this study, the covariance analysis was used to analyze the data. Meanwhile, the data were analyzed via the SPSS software, version 22.
Study instruments
Psychological resilience questionnaire
The Dennis and Vanderwall psychological resilience questionnaire was designed in 2010 [30]. This questionnaire included 20 questions to measure a type of psychological flexibility that is necessary for a person’s success to challenge and replace ineffective thoughts with more efficient ones and has 3 subscales of alternatives, control, and alternatives for human behavior. This questionnaire is based on a 7-point Likert scale ranging from 1 (completely disagree) to 7 (completely agree). The range of questionnaire scores is from 20 to 140. Higher scores indicate greater psychological flexibility. The cut-off score for this questionnaire is 70. In the research by Dennis and Vanderwaal, the concurrent validity of this questionnaire with the Beck depression questionnaire was - 0.39, and its convergent validity with the psychological flexibility scale of Martin and Robin was 0.75 [30]. Masuda and Tali also calculated the reliability of this questionnaire at 0.82 [31]. The reliability of this questionnaire in the Ali Akbari Dehkordi et al. study was obtained at 0.79 using the Cronbach α coefficient [18].
Connor and Davidson resilience questionnaire
Connor and Davidson designed the resilience questionnaire in 2003 to measure the level of resilience in different people [32]. This scale is self-reported and has 25 questions. The scoring of this scale is based on a Likert scale ranging from 0 (completely false) to 4 (always true). To obtain the total score of the questionnaire, the total scores of all the questions are added together. This score ranges from 0 to 100. Higher scores indicate greater resilience of the respondent. The cut-off point for this questionnaire is 50; that is, a score higher than 50 indicates people who have higher resilience, and higher scores demonstrate a higher level of resilience. The reliability (by re-test method and Cronbach α) and validity (by factor analysis, convergent, and divergent validity) have been verified in different groups (normal and at risk). Connor and Davidson reported the Cronbach α coefficient of the resilience scale at 0.89. Also, the reliability coefficient obtained from the re-test method in a 4-week interval was 0.87. Khoshnazari, Hosseini, Falahi Khoshkotab, and Bakhshi translated the resilience questionnaire and reported its content validity as 0.84 and its reliability coefficient as 0.94 [33]. In addition, the Cronbach α in the present study was 0.86.
Measurement of blood sugar factor: In this research, the fasting ELISA method was used to measure this factor in diabetic patients using a laboratory kit in the pre-test and post-test stages.
Results
The demographic findings showed that the mean age of the participants in the experimental group was 47.9 years while the control group was 49.3 years. Also, 46.2% of the participants had a diploma, 35.2% had a bachelor’s degree, and 18.6% had a postgraduate degree. Among the participants, 84.1% were married and 15.9% were single. The Mean±SD of the research variables are presented in Table 2.
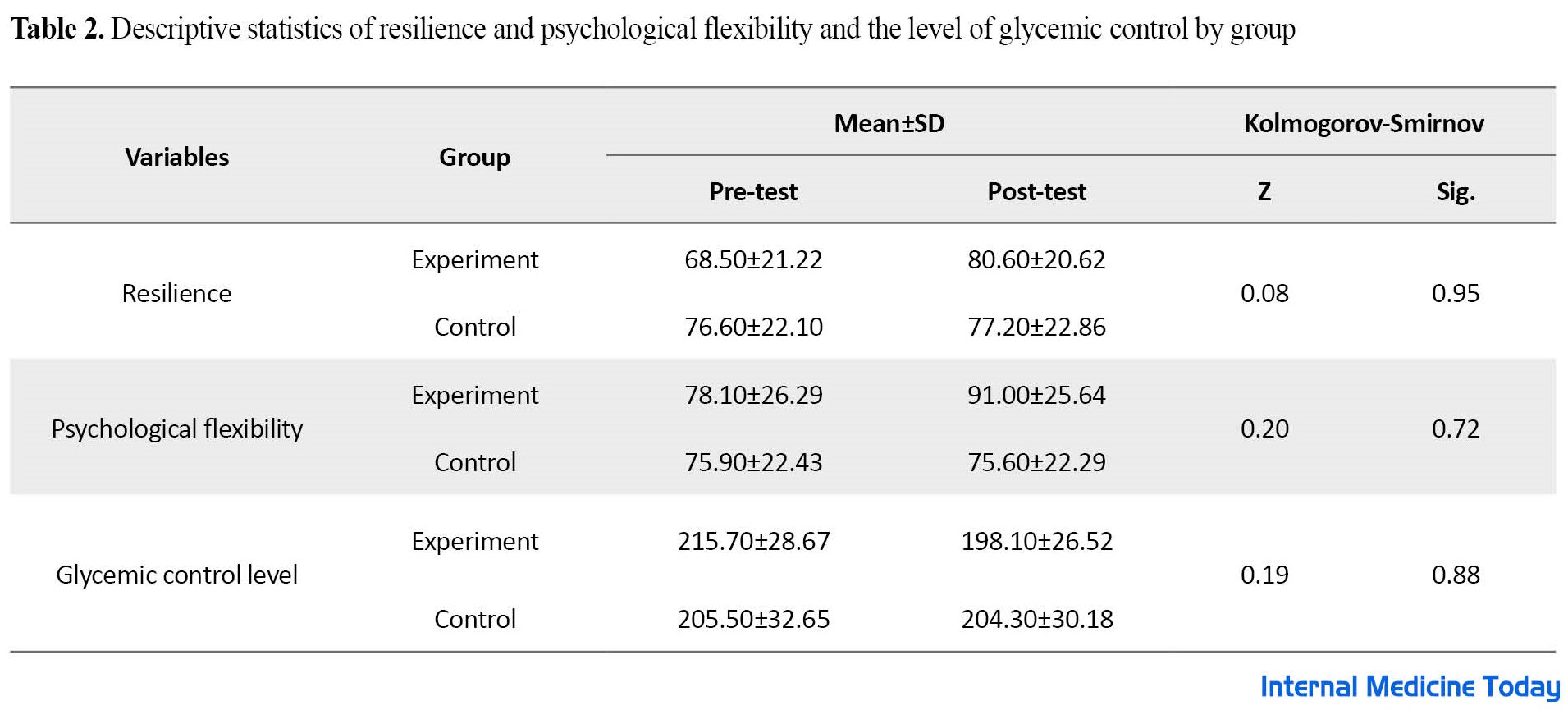
Table 2 shows the Mean±SD of the variables of resilience and psychological flexibility and the level of glycemic control in the pre-test and post-test phases. The results showed a significant difference in the scores of the experimental group after dialectical behavior therapy. Also, the Kolmogorov-Smirnov test shows that the assumption of normality is established for all variables of resilience, psychological flexibility, and the level of glycemic control (P<0.05). The results of the Lon test showed that the assumption of homogeneity of variance was also valid for all variables of resilience (F=0.262, P=0.615), psychological flexibility (F=1.45, P=0.243), and glycemic control (F=0.409, P=0.530). The results of multivariate covariance analysis are reported in Table 3
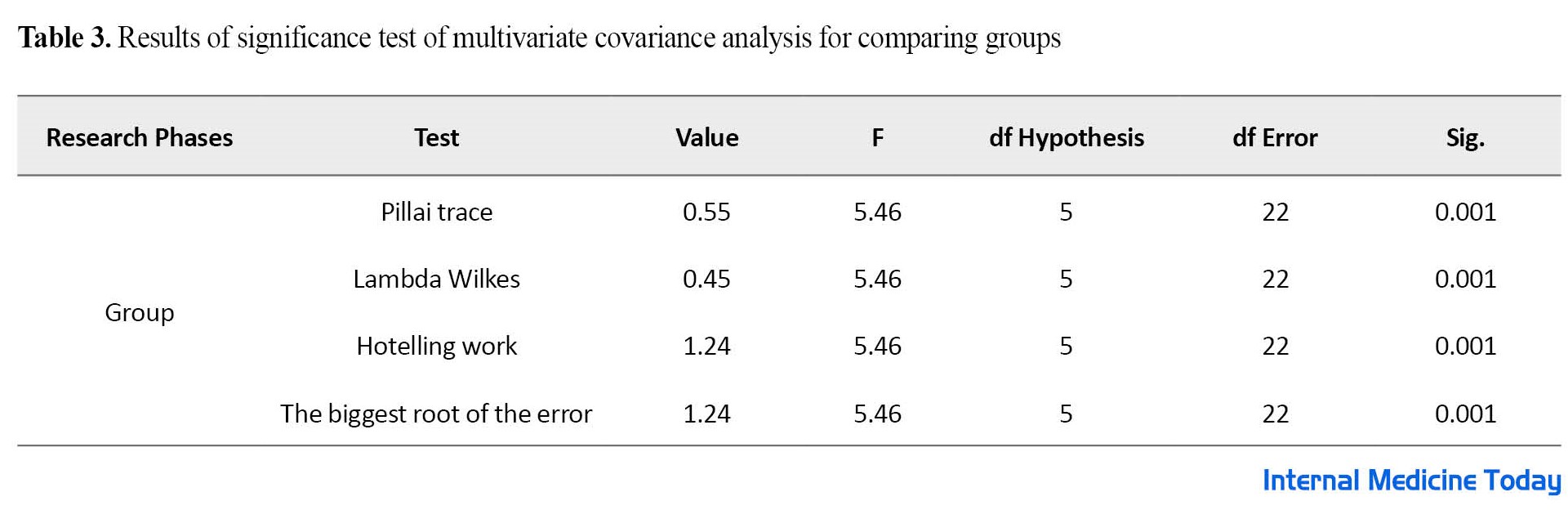
According to Table 3, the results of the multivariate covariance analysis indicate that the F obtained in all tests is significant at P<0.05 level with degrees of freedom at 5 and 22. The results showed a significant difference in the research variables after removing the pre-test effect, P<0.05 and (df=5 and df=22) and (F=5.46 and Pillai trace=0.55). In the following, univariate analysis of the covariance test was used for a more detailed understanding and investigation of the separate effect of the independent variable on the dependent variables.
The results of Table 4 show a significant difference between the two experimental and control groups in the variables of resilience, psychological flexibility, and the amount of glycemic control (P<0.001).
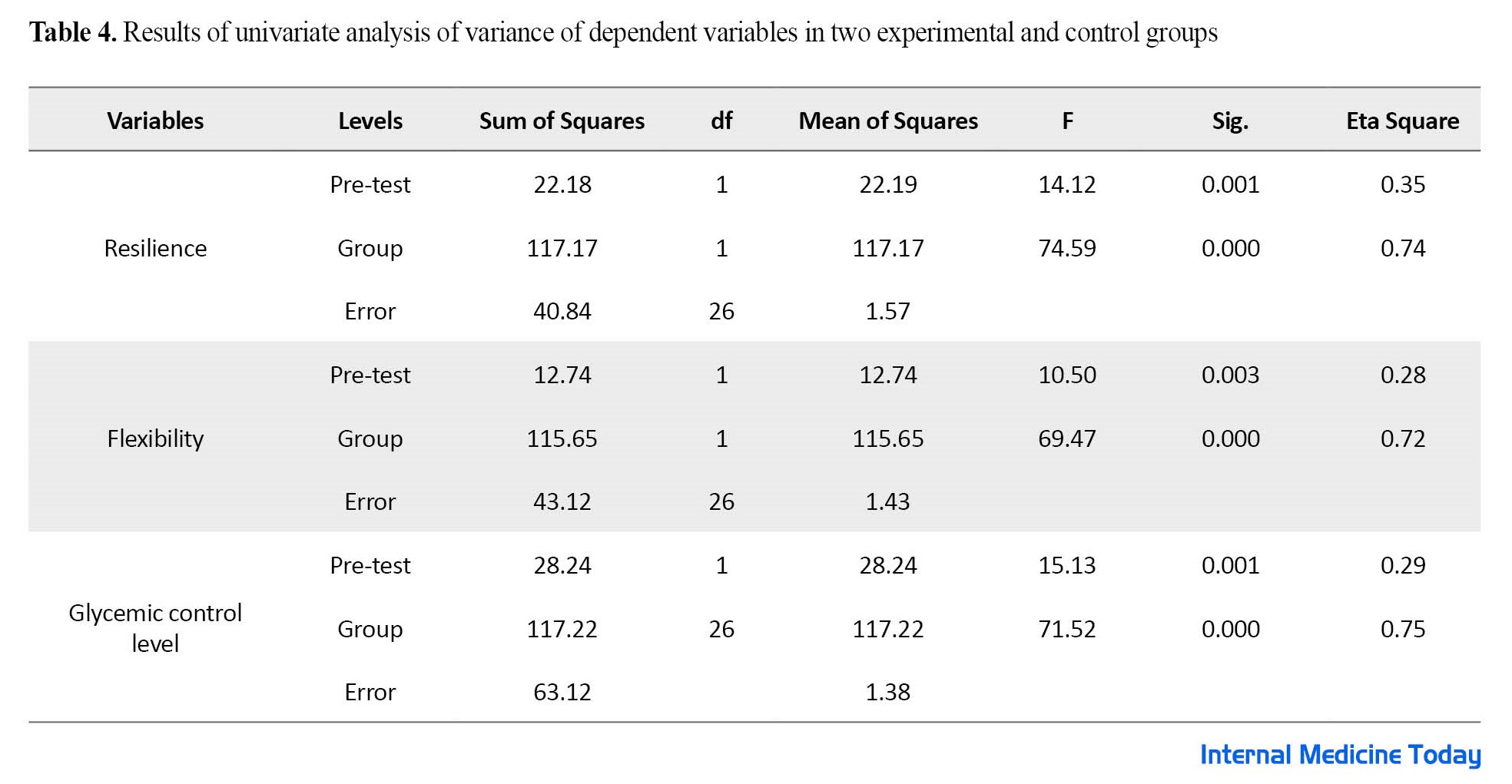
The obtained Eta coefficient indicates that the variance related to the difference between the two groups in the post-test is because of the effectiveness of dialectical behavior therapy.
Discussion
This research was conducted to investigate the effectiveness of dialectical behavior therapy on the resilience, flexibility, and glycemic control of diabetic patients. The findings showed that dialectical behavior therapy is effective in increasing resilience, flexibility, and glycemic control in patients. This finding is in line with the results of other studies [21, 25-29].
In explaining this finding, patients are taught various behavioral therapy skills concerning resilience to solve problems, social support, optimism, tolerance of chaos, purposefulness and hope, and having an enjoyable life. A dialectic that includes basic comprehensive awareness, distress tolerance, emotion regulation, and efficiency between individuals was taught and its practical practice was discussed in a group session. Dialectical therapy by using communication skills, self-awareness, problem-solving, behavior control, asking for help, optimism, eliminating misconceptions, empathy, and decision-making power can increase hopeful and purposeful thinking in patients, thereby improving mental health and helping improve resilience skills [27]. In a more specific way, due to the characteristics and chronic nature of diabetes, accepting the sufferings and bearing the disturbances caused by diabetes is very vital in the resilience of these people; therefore, teaching the skills of coping with disturbance has been effective in this group by improving the level of pain tolerance caused by living with diabetes and preventing it from turning into psychological suffering. On the other hand, since dialectical behavior therapy has placed mindfulness at the center of its work, it can be effective in promoting resilience by increasing the individual’s focus and teaching life in the present moment, and adopting a non-judgmental approach. Emotional regulation training has been effective in promoting resilience through reducing emotional vulnerability and learning methods to reduce negative vulnerability and increase emotional toughness [28].
The main core of dialectical behavior therapy is mindfulness and emotional regulation skills that teach patients to be aware of their emotions, thoughts, and behaviors, to face emotions, and to act against strong emotional desires (increasing cognitive flexibility). In addition, practicing non-fusion of thought and excitement is effective for regulating emotions and reducing instability and impulsivity [24]. Therefore, through dialectical behavior therapy and the techniques and skills a person becomes aware of the impact of the relationship between thoughts and emotions, and automatic maladaptive evaluation is identified, and this cognitive re-evaluation will increase flexibility in thinking. Doing mindfulness exercises by increasing an individual’s ability to turn their attention from what is not useful or effective (such as focusing on negative thoughts) to what is useful and effective can help to moderate their emotional experience [21], which makes people with diabetes have more cognitive flexibility, based on which they find alternatives to difficult situations, find difficult situations controllable, and find meaning and positive alternatives for other subject’s events and social behaviors [18]. Accordingly, dialectical behavior therapy can reduce psychological damage, such as anxiety and variables by creating the ability to tolerate disturbance and create more psychological peace. Also, dialectical behavior therapy as a supportive treatment that requires a strong relationship between the patient and the therapist can develop skills such as tolerance of helplessness, mindfulness, self-regulation of emotions, and efficient skills in patients by providing new strategies to moderate the effects of uncomfortable conditions and increasing psychological flexibility, it helps patients with diabetes to cope with the painful experiences of diabetes [15].
Conclusion
The results of the research showed that dialectical behavioral therapy skills, such as distress tolerance, emotion regulation, and interpersonal efficiency led to an increase in resilience and psychological flexibility in patients with diabetes. The present research was conducted on diabetic patients of Gorgan City, Iran. Therefore, if there is a change in the number and gender of the population and the statistical sample, different results may be obtained. It is suggested that this research be conducted as a case study in several statistical populations (cardiovascular patients, other cities, women, and men) and the results be compared with each other. It is suggested that policymakers in the field of health and treatment try to increase the resilience and flexibility of diabetic patients through various methods such as dialectical behavior therapy.
Ethical Considerations
Compliance with ethical guidelines
This project approved by received the the Research Vice-Chancellor of Payam-e-Noor University (Code: IR.PNU.REC.1401.024).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors' contributions
The both authord contributed equally to the writing of the article.
Conflicts of interest
The authors declared no conflict of interest.
Acknowledgements
All authors thank all the participants for their cooperation in this research.
References
- Agha Yousefi A, Safari Y, Ahmadi S, Abbaspour P. [Studying the effectiveness of coping therapy on psychological markers (stress, quality of life and coping strategies) in type II diabetic patients (Persian)]. Scientific-Research Quarterly of Health Psychology. 2020; 9(34):25-40. [Link]
- Rajabi M, Malehi al-Zhakrini S, Asadi J, Mirzaei M. [The effectiveness of metacognitive training on cholesterol (LDL), cholesterol (HDL) and depression in patients with type 2 diabetes (Persian)]. Health Psychology. 2020; 9(36):87-104. [Link]
- Rezai Kokhdan F, Dartaj F, Ghaemi F, Hatami M, Delavar A. [Comparing the effectiveness of mindfulness and cognitive behavioral therapy on blood sugar and glycosylated hemoglobin in type 2 diabetes patients (Persian)]. The Medical Journal of Mashhad University of Medical Sciences. 2020; 63(3):2414-27. [Link]
- Zimmet P, Alberti KG, Magliano DJ, Bennett PH. Diabetes mellitus statistics on prevalence and mortality: Facts and fallacies. Nature reviews. Endocrinology. 2016; 12(10):616-22. [DOI:10.1038/nrendo.2016.105] [PMID]
- Fakhri M, Bahar A, Amini F. [Effectiveness of mindfulness on happiness and blood sugar level in diabetic patients (Persian)]. Journal of Mazandaran University of Medical Sciences. 2017; 27(151): 94-104. [Link]
- Carpenter R, DiChiacchio T, Barker K. Interventions for self- management of type 2 diabetes: An integrative review, International Journal of Nursing Sciences. 2018; 6(1):70-91. [DOI:10.1016/j.ijnss.2018.12.002] [PMID] [PMCID]
- Srinivasan BT, Davies M. Glycaemic management of type 2 diabetes. Medicine. 2019; 47(1):32-9. [DOI:10.1016/j.mpmed.2018.10.009]
- Meerow S, Newell JP. Urban resilience for whom, what, when, where, and why? Urban Geography. 2019; 40(3):309-29. [DOI:10.1080/02723638.2016.1206395]
- Gultekin A, Kavak F, Ozdemir A. The correlation between spiritual well-being and psychological resilience in patients with liver transplant. Medicine Science. 2019; 8(3):531-6. [DOI:10.5455/medscience.2018.07.8997]
- Iacoviello M, Charney DS. Cognitive and behavioral components of resilience to stress. In: Chen A, editor. Stress resilience. Massachusetts: Academic Press; 2020. [DOI:10.1016/B978-0-12-813983-7.00002-1]
- Zain Abadi H, Khabareh K. [A reflection on the phenomenon of a resilient teacher; Phenomenology of teachers’ attitudes and lived experiences (Persian)]. Management and Planning in Educational Systems. 2020; 13(1):13-36. [DOI:10.29252/mpes.13.1.13]
- Golestane M, Timuri E. [Investigating some of the important antecedents and consequences of teachers’ resiliency (Persian)]. Psychological Achievement. 2019; 26(1):169-90. [Link]
- Hosseini S, Ahadi M, Hatami M, Khalatbari J. [Comparison of the effectiveness of mindfulness-based therapy and acceptance and commitment therapy on resilience, psychological well-being and blood sugar levels in patients with type 2 diabetes (Persian)]. Iranian Journal of Psychiatric Nursing. 2021; 9(1):89-102. [Link]
- Sadeghi M, Safari Mousavi S, Farhadi M. [The role of psychological flexibility and self-compassion in predicting depression, anxiety and stress in patients with type 2 diabetes (Persian)]. Journal of Isfahan Medical School, 2016; 35(452):1468-75. [Link]
- Deledda G, Giansante M, Poli S, Geccherle E, Fantoni G, Scandola M, et al. The role of psychological flexibility in cancer pain. Journal of Psychosomatic Research. 2018; 109:98. [DOI:10.1016/j.jpsychores.2018.03.044]
- Wang S, Zhou Y, Yu S, Ran L, Liu XP, & Chen YF. Acceptance and Commitment therapy and cognitive-behavioral therapy as treatments for academic procrastination: A randomized controlled group session. Research on Social Work Practice. 2017; 27(1):48-58. [DOI:10.1177/1049731515577890]
- Igarashi Y, Staples J, Vigil S, Pero G, Gardner R, Thomat A, et al. The impact of psychological flexibility in the relationship between discrimination and internalized transnegativity among transgender and gender expansive adults. Journal of Contextual Behavioral Science. 2022; 24:42-50. [DOI:10.1016/j.jcbs.2022.03.005]
- Ali Akbari Dehkordi M, Ghafouri S, Jafari F, Mohteshmi T. [The effectiveness of education based on acceptance and commitment on physical symptoms, psychological flexibility and social health of patients with psoriasis (Persian)]. Knowledge and Research in Applied Psychology. 2019; 21(4):118-32. [DOI:10.30486/JSRP.2019.580247.1584]
- Dheer R, Lenartowicz T. Cognitive flexibility: Impact on entrepreneurial intentions. Journal of Vocational Behavior. 2019; 115:103339. [DOI:10.1016/j.jvb.2019.103339]
- Watts R, Luoma JB. The use of the psychological flexibility model to support psychedelic assisted therapy. Journal of Contextual Behavioral Science. 2020; 15:92-102. [DOI:10.1016/j.jcbs.2019.12.004]
- Khakshor Shandiz F, Shahabizadeh F, Ahi Q, Mujahidi M. [The effectiveness of dialectical behavior therapy on stress and cognitive flexibility of women with type 2 diabetes (Persian)]. Journal of Qom University of Medical Sciences. 2021; 15(5):358-67. [DOI:10.32598/qums.15.5.2373.1]
- Arabzadeh A, Nemati M, Turkman Menesh A, Faramarzi F. [The effectiveness of dialectical behavior therapy on increasing self-compassion and psychological well-being and decreasing blood pressure in individuals with substance abuse (Persian)]. Scientific Quarterly of Research on Addiction. 2022; 15(62):261-88. [DOI:10.52547/etiadpajohi.15.62.261]
- Flynn D, Kells M, Joyce M. Dialectical behaviour therapy: Implementation of an evidence - based intervention for borderline personality disorder in public health systems. Current Opinion in Psychology. 2021; 37:152-7. [DOI:10.1016/j.copsyc.2021.01.002] [PMID]
- Kim H, Yeo J. Impact of sexual attitude and marital intimacy on sexual satisfaction in pregnant couples: An application of the actor -partner interdependence model. Korean Journal of Women Health Nursing. 2017; 23(3):201. [DOI:10.4069/kjwhn.2017.23.3.201]
- Cohen J, Norona JC, Yadavia JE, Borsari B. Affirmative dialectical behavior therapy skills training with sexual minority veterans. Cognitive and Behavioral Practice. 2021; 28(1):77 -91. [DOI:10.1016/j.cbpra.2020.05.008]
- Mitchell R, Roberts R, Bartsch D, Sullivan T. Changes in mindfulness facets in a dialectical behavior therapy skills training group program for borderline personality disorder. Journal of Clinical Psychology. 2019; 75(6):958 -69. [DOI:10.1002/jclp.22744] [PMID]
- Bahrami F, Zahedi Y. [The effectiveness of group dialectical behavioral therapy on increasing the life expectancy and resilience of exceptional children's mothers (Persian)]. Culture of Counseling and Psychotherapy. 2018; 9(35):171-89. [Link]
- Ramaiya MK, McLean C, Regmi U, Fiorillo D, Robins CJ, Kohrt BA. A dialectical behavior therapy skills intervention for women with suicidal behaviors in rural Nepal: A single- case experimental design series. Journal of Clinical Psychology. 2018; 74(7):1071-91. [DOI:10.1002/jclp.22588] [PMID] [PMCID]
- Lee S, Mason M. Effectiveness of brief DBTinformed group therapy on psychological resilience: A preliminary naturalistic study. Journal of College Student Psychotherapy. 2019; 33(1):25-37. [DOI:10.1080/87568225.2018.1425646]
- Dennis J, Vander Wal J. The cognitive flexibility inventory: Instrument development and estimates of reliability and validity, Cognitive Therapy Research. 2010; 34(1):241-53. [DOI: 10.1007/s10608-009-9276-4]
- Masuda A, Tully EC. The role of mindfulness and psychological flexibility in somatization, depression, anxiety, and general psychological distress in a nonclinical college sample. Journal of Evidence-Based Complementary & Alternative Medicine. 2012; 17(1):66-71. [DOI:10.1177/2156587211423400]
- Connor KM, Davidson JR. Development of new resilience scale: The Connor- Davidson, Resilience scale (CD-RISC). Journal of Depression and Anxiety. 2003; 18(2):76- 82. [DOI:10.1002/da.10113] [PMID]
- Rahimpour S, Arefi M, Manshai G. [Effectiveness of integrated training of time perspective and mindfulness on resilience and wisdom (Persian)]. Research Paper on Positive Psychology. 2021; 7(1):35-52. [DOI:10.22108/PPLS.2021.118779.1798]
Type of Study: Applicable |
Subject:
Mental Health
Received: 2022/10/16 | Accepted: 2022/09/23 | Published: 2022/09/23
Received: 2022/10/16 | Accepted: 2022/09/23 | Published: 2022/09/23
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





