

Volume 27, Issue 4 (Autumn 2021)
Intern Med Today 2021, 27(4): 466-485 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nikfarjam M, Khosravi N, Ganji F, Parvin N, Goodarzi I, Mohammadi-ahmadmahmoudi A. Exploring the Impact of Teaching Reading, Writing, and Math on the Mental State of Schizophrenic Patients. Intern Med Today 2021; 27 (4) :466-485
URL: http://imtj.gmu.ac.ir/article-1-3606-en.html
URL: http://imtj.gmu.ac.ir/article-1-3606-en.html
Masoud Nikfarjam1 

 , Najmeh Khosravi *2
, Najmeh Khosravi *2 

 , Forouzan Ganji3
, Forouzan Ganji3 

 , Neda Parvin4
, Neda Parvin4 

 , Iraj Goodarzi1
, Iraj Goodarzi1 

 , Abdollah Mohammadi-ahmadmahmoudi1
, Abdollah Mohammadi-ahmadmahmoudi1 




 , Najmeh Khosravi *2
, Najmeh Khosravi *2 

 , Forouzan Ganji3
, Forouzan Ganji3 

 , Neda Parvin4
, Neda Parvin4 

 , Iraj Goodarzi1
, Iraj Goodarzi1 

 , Abdollah Mohammadi-ahmadmahmoudi1
, Abdollah Mohammadi-ahmadmahmoudi1 


1- Department of Psychiatry, School of Medicine, Shahrekord University of Medical Sciences, Shahrekord, Iran.
2- Student Research Committee, Shahrekord University of Medical Sciences, Shahrekord, Iran. ,najmehk776@gmail.com
3- Department of Community Medicine, Social Determinants of Health Research Center, School of Medicine, Shahrekord University of Medical Sciences, Shahrekord, Iran.
4- Department of Nursing, School of Nursing & Midwifery, Shahrekord University of Medical Sciences, Shahrekord, Iran.
2- Student Research Committee, Shahrekord University of Medical Sciences, Shahrekord, Iran. ,
3- Department of Community Medicine, Social Determinants of Health Research Center, School of Medicine, Shahrekord University of Medical Sciences, Shahrekord, Iran.
4- Department of Nursing, School of Nursing & Midwifery, Shahrekord University of Medical Sciences, Shahrekord, Iran.
Full-Text [PDF 5245 kb]
(1519 Downloads)
| Abstract (HTML) (4324 Views)
Full-Text: (5279 Views)
1. Introduction
Schizophrenia has a low prevalence, but aging and population growth have increased patients and disease costs [1]. In general, the symptoms are divided into two main categories. Positive symptoms include hallucinations, delusions, and formal thought disorders, and negative symptoms are anhedonia, alogia, and avolition [2]. Although schizophrenia is not a cognitive disorder, it often results in the destruction of cognitive domains [3]. Cognitive deficits in patients with schizophrenia affect and limit all aspects of life, including activities of daily living, job performance, education, parenting, self-care, interpersonal relationships, independent living, and leisure [4]. Timely and proper treatment can prevent many complications of this disease. There are effective treatments for this disorder, but patients and their families often lack access to good care, and new treatment strategies are needed [5]. Although current therapies include antipsychotics along with psychological therapies and social support, modern and complementary therapies should be sought with minimal complications and low costs [6, 7].
Reading and writing skills are poor among patients with mental disorders. On the other hand, there has been poor performance in these patients’ previous education status [8, 9]. In addition to improving mental status, these skills can facilitate the treatment process for patients [10, 11]. Patients with schizophrenia show severe problems with reading ability, which is a potentially repairable cause of socioeconomic dysfunction. These defects are not currently recorded during routine clinical evaluation of patients. These disorders help reduce schizophrenia-related educational and job performance [12]. In addition, in some cases, schizophrenia becomes resistant to treatment, and this situation characterizes by treatment failing with two antipsychotic drugs for at least six weeks. Even in some cases, up to 30% of schizophrenia patients poorly responded to psychiatric medications, and about 7% have no response at all [2]. Among the methods used to treat cognitive and mental disorders is teaching math and improving learning skills. Mathematic solving skills can improve attention, self-efficacy, and memory disorders. Mathematics reduces cognitive problems by activating and developing individuals’ cognitive domains and controlling emotional and behavioral behaviors [13, 14, 15]. Therefore, considering the importance of literacy in solving the daily problems and social needs of schizophrenic patients and their possible impact on their positive and negative symptoms, and given that no study has been performed in this area, we decided to determine the effect of reading, writing, and mathematics education on the mental status of schizophrenic patients.
2. Materials and Methods
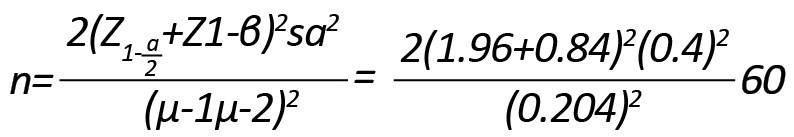
This double-blind clinical trial study was performed on patients with schizophrenia admitted to Sina Junqan Hospital (located in Chaharmahal and Bakhtiari Province in southwestern Iran) in 2015. The samples were recruited by a simple sampling method. The sample size was estimated at 30, with a 95% confidence level, and 80% power using the following formula. So there are 30 patients in the control and intervention groups, and a total of 60 samples in this study participated.
Patients were randomly divided into two groups: patients under routine treatment (control group) and patients under routine treatment with educational intervention (intervention group). Initially, there were 30 participants in each control and intervention group, but eventually, 24 patients remained in the control group and 23 in the intervention group (Figure 1). The inclusion criteria were as follows: a record of hospitalization, 15-60 years old, ability to write (lacking specific physical disabilities), no mental retardation, not being in the acute phase of illness, understanding Persian language, no visual impairment, head injury, Alzheimer disease, and addiction. Illness, addiction, and unwillingness to continue the study were considered the exclusion criteria. Eligible individuals were selected based on their educational status, positive and negative symptoms. The subjects with similar status were identified for the mentioned parameters and were randomly divided into control and intervention groups. The study data were collected using a demographic information checklist (including age, gender, education level), Anderson’s positive and negative symptoms questionnaire, and the mini-mental state examination.
Anderson’s positive and negative symptoms questionnaire is a standard instrument used in various studies in Iran. The positive symptoms section includes hallucination, delusion, bizarre behavior, and thought disorders. The choices to answer the items are non-suspicious with a score of 0-1, mild to moderate with a score of 2-3, and severe to the extreme with a score of 4-5. Higher scores indicate more severe symptoms in the respondent. The negative symptoms include affective blunting, alogia, avolition, anhedonia, social indifference, and inattention. They are rated on the same scale of positive symptoms [16, 17]. In a study in Iran, Ghamari Givi et al. reported the Cronbach α value of 0.78 for the questionnaire, and its validity was reported acceptable by exploratory factor analysis [18]. In the study of Khalaf Beigi et al., the Cronbach α value was obtained 0.78 for the negative symptoms and 0.77 for the positive symptoms [16].
The Mini-Mental State Examination (MMSE) questionnaire measures mental status. It has been translated into Persian and measures a person’s cognitive functions, including orientation, registration, attention and calculation, recent memory, and various language functions. This questionnaire has been translated into Persian and includes 19 items in various fields that measure cognitive status, with minimum and maximum possible scores of 0 to 30, respectively. Scores 25-30 indicate normal cognitive status, 20-24 possible cognitive impairment, and >19 indicate definite cognitive impairment [19]. The MMSE has also been used in Iran. For example, Seyedian et al. showed the acceptable validity and reliability of the instrument and reported the Cronbach α coefficient of 0.81 for the whole test [20].
In the intervention group, reading, writing, and math skills were taught simultaneously. Group sessions were conducted by a trained person for a maximum of 1 hour, three sessions per week. Group meetings included six to eight patients. These sessions lasted for 6 months, and at the completion of the third month, positive and negative symptoms questionnaire and the MMSE were administered to patients. During the class, the patients were categorized, and the content of the courses was selected based on a preliminary examination of patients who had previously been identified.
Because of the importance of communication for these patients, in the reading skills sessions, the trainer presented frequently used words and keywords to communicate, social conversations, meeting of social needs, and also a review of the alphabet at the beginning of the session. After ensuring learning of the vocabulary in the form of textbooks in preschool and elementary school, if patients were to progress academically, their reading comprehension skills would be reviewed. In the math lesson, after getting acquainted with the concept of numbers and related items based on preschool and first-grade content, special skills of problem-solving related to social life skills such as shopping, giving money, keeping time, and calculating distance were also taught. As with group meetings, at the beginning of each session, a review of the previous sessions and then at the end, a summary and review of the new lesson was accomplished. In addition, some exams were administered every two weeks.
After each session, the patients were given assignments for subsequent sessions. The class style was in the form of a purposeful group led by the teacher and the patients’ participation.
In addition to the beginning of the course, at the completion of the 6 months intervention, the positive and negative symptoms questionnaire and patients’ cognitive status were retested. It should be noted that at the beginning of the first class session, the class regulations were explained to the participants. In the control group, patients received routine treatments and did not undergo training. During treatment, the patients were kept as similar as possible in terms of treatment conditions, such as medication and psychology. In addition to the textbooks mentioned, some contents were determined for training in the last month by the research team and the cooperation of psychologists and physicians. These contents were taught to the patients. In addition, patients were given information about the disease, treatment, follow-up, and related issues throughout this month (by a fellow psychologist).
To strengthen the appropriate behaviors of patients during the class and in addition to their academic progress, positive reinforcement was done by giving prizes throughout the course.
The obtained data were analyzed in SPSS18 using descriptive statistics of central and dispersion indexes (mean and standard deviation) and inferential statistics of the Kolmogorov-Smirnov test and repeated measures Analyses of Variance (ANOVA). In addition, the non-parametric Mann-Whitney test was performed with a significance level of P <0.05 due to the non-normal distribution of samples.
3. Results
In this study, 47 patients with schizophrenia were assigned into two groups of 24 controls (routine therapies) and 23 cases (reading, writing, and math education and routine therapies). The Kolmogorov-Smirnov test showed that the data were normally distributed. Two groups did not show a statistically significant differences regarding age (P=0.26), gender (P=0.059), and the education level (P=0.1). Most samples in both groups had elementary education. In general, the two groups were matched in terms of age, sex, and level of education (Table 1).
.jpg)
In the two groups, the scores of positive and negative symptoms and their dimensions and MMSE in 3 stages of the study, i.e., the first time (before the intervention), second time (third months after the intervention), and third time (sixth months after the intervention) are shown in Tables 2 and 3.
.jpg)
.jpg)
In this study, the overall score of positive symptoms (P=0.038), hallucinations (P=0.033), delusions (P=0.023), and formal positive mental disorder (P=0.029) in the third time in the intervention group was significantly lower than the control group (Table 2). Also, in the case of negative symptoms, in the third time measurement, the affective blunting in the intervention group was significantly lower than the control group (P=0.039). The MMSE scores were reported for the third time in the intervention group, which were more and better than the control group (P=0.013).
Based on the findings of repeated measures AVOVA, changes in the overall score of positive symptoms and all its dimensions were statistically significant and decreased in the intervention group (P<0.001), but in the control group, only changes in positive thought disorder (P=0.031) and bizarre behaviors (P<0.001) were significant. Regarding the changes in the score of the first and third month of positive symptoms, the findings showed that the difference between the score of the first and third times in the total score of positive symptoms and all its dimensions is significantly different between the two groups (P<0.05) (Table 2).
Based on the findings of repeated measures ANOVA, changes in the overall score of negative symptoms and all its dimensions were statistically significant and decreased in the intervention group (P<0.001), except for alogia compared to the control group (P=0.124). The rest of the dimensions were significant. Also, the MMSE was reported in both control and intervention groups (P<0.05). Regarding negative symptoms, there is a significant difference between the two groups in the scores of the first and third times in the overall score of negative symptoms and some of its dimensions, including affective blunting and alogia (P<0.05). The difference between the scores of the first and third times of the short mental status test was also reported significant between the two groups (P<0.05) (Tables 2 and 3).
Changes in the MMSE score also were significant in both intervention (P=0.002) and control (P=0.017) groups, but in comparison between the two groups, this rate was higher in the intervention group after the sixth month (Table 4).

4. Discussion
The current study was conducted to investigate the effect of reading, writing, and math education on the mental state of schizophrenic patients. In this study, the overall scores of positive symptoms, hallucinations, delusions, and formal positive thought disorder were lower in the third time (After six months of intervention) measurement in the intervention group compared to that in the control group. In the case of negative symptoms, in the third measurement, the affective blunting was significantly lower in the intervention group than in the control group. The standard schizophrenia treatment based on biological, psychological, and social models includes the administration of antipsychotic drugs, psychological interventions, and social and family support [21]. In general, there is extensive evidence of the effectiveness of life skills training on social, cognitive, and emotional functioning in patients with schizophrenia [22].
Research has shown that life skills training, including social skills, is associated with improved patient cognitive function, especially in terms of verbal ability, information processing speed, and memory.
Some research has shown that these kinds of training increase problem-solving skills, the quality of conversational skills, cognitive interactions, positive symptoms, long-term visual memory, self-expression, and communication with others while reducing relapse periods [22, 23, 24, 25]. On the other hand, reading, writing, and math training are cognitive in nature, which is related to their effect on the psychological symptoms of patients with schizophrenia. One study showed that poetry, storytelling, and other texts had a great impact on improving patient interactions, reducing impulsivity, increasing realism, improving self-care, interpersonal relationships, and increasing patient participation [26].
In their study of 82 patients with schizophrenia, Aubin et al. found significant relationships between performance and visual-spatial learning, spatial memory, and negative symptoms in patients with schizophrenia [27]. A study by Steel et al. showed that positive memory training protocol was an effective, inexpensive, and convenient method, and because the dominant focus of the intervention was on past positive experiences, the patient’s involvement would be high [28].
In the current study, the changes in the MMSE score were significant in both the intervention and control groups. In the third time (6 months after the intervention), the scores were higher in the intervention group. Greiq et al. conducted a one-year study of neuro-cognitive therapy to identify cognitive impairments in patients with schizophrenia who had participated in an occupational therapy program. That study included computer cognitive training exercises. One year after treatment, patients receiving neurological and occupational therapy showed significant improvements in executive functions and working memory compared to patients who had only undergone occupational therapy [29]. A review study also showed that science learning and memory enhancement could potentially enhance cognitive function, increase attention, increase drug effectiveness, and reduce symptoms and duration of illness in people with schizophrenia [30]. For other neuropsychiatric disorders, studies have also been conducted on the effectiveness of teaching skills, such as reading and writing, and math. In this regard, a study was conducted to teach basic concepts and strengthen the ability to read and write on the patient undergoing the intervention. Statistical analysis showed that the intervention group attained sufficient skills of reading and writing, and the cognitive intervention improved cognitive function in the intervention group [31]. Another study also showed that reading, writing, math, and content interventions improve the behavioral and academic outcomes of students with emotional and behavioral disorders. This training had positive outcomes for students’ symptoms and academic achievement and improved their cognitive processes [32]. Thus, schizophrenia, which is often associated with cognitive impairment such as objective thinking, information processing disorder, impaired social and occupational activity, impaired social cognition, impaired interpersonal relationships, and low responsibility, can be partially addressed by teaching a variety of life skills to reduce existing deficiencies. Teaching these skills helps the patient to cope with the positive symptoms of their illnesses through acquiring the self-management skills of the negative symptoms learning how to communicate verbally and non-verbally with others, and making appropriate emotional statements. Eventually, the patients will be able to partly control social anxiety and avoidance behaviors by learning how to communicate with others in different situations (through role-playing and role modeling).
Therefore, learning social and life skills has led to the patients’ self-help and their active participation in controlling the symptoms of illness and the development of self-management skills. In this way, the patients gain better insight into their condition, leading to greater acceptance of responsibility for their behaviors [33].
Learning to read and write and math exercises can be effective in improving the positive and negative symptoms of patients with schizophrenia and improving their cognitive symptoms.
However, it is recommended that these methods be used in addition to conventional therapies to improve patients’ cognitive status as a complementary treatment in the health and rehabilitation centers. It is recommended that future studies be conducted with larger sample size and compare this treatment with other types of cognitive therapies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Shahrekord University of Medical Sciences (Code: IR.SKUMS.REC.91-5-4).
Funding
This study was extracted from a research project approved by the Deputy of Research and Technology of Shahrekord University of Medical Sciences (No. 1150).
Authors' contributions
Study design, and writing of the manuscript: Masoud Nikfarjam and Najmeh Khosravi; Data collection: Neda Parvin; Data analysis and initial review: Forouzan Ganji; Preparation and final approval of manuscript: Iraj Goodarzi, Abdollah Mohammadi-ahmadmahmoudi, Masoud Nikfarjam, Najmeh Khosravi, Forouzan Ganji, and Neda Parvin.
Conflicts of interest
The authors declared no conflict of interest.
Refrences
Schizophrenia has a low prevalence, but aging and population growth have increased patients and disease costs [1]. In general, the symptoms are divided into two main categories. Positive symptoms include hallucinations, delusions, and formal thought disorders, and negative symptoms are anhedonia, alogia, and avolition [2]. Although schizophrenia is not a cognitive disorder, it often results in the destruction of cognitive domains [3]. Cognitive deficits in patients with schizophrenia affect and limit all aspects of life, including activities of daily living, job performance, education, parenting, self-care, interpersonal relationships, independent living, and leisure [4]. Timely and proper treatment can prevent many complications of this disease. There are effective treatments for this disorder, but patients and their families often lack access to good care, and new treatment strategies are needed [5]. Although current therapies include antipsychotics along with psychological therapies and social support, modern and complementary therapies should be sought with minimal complications and low costs [6, 7].
Reading and writing skills are poor among patients with mental disorders. On the other hand, there has been poor performance in these patients’ previous education status [8, 9]. In addition to improving mental status, these skills can facilitate the treatment process for patients [10, 11]. Patients with schizophrenia show severe problems with reading ability, which is a potentially repairable cause of socioeconomic dysfunction. These defects are not currently recorded during routine clinical evaluation of patients. These disorders help reduce schizophrenia-related educational and job performance [12]. In addition, in some cases, schizophrenia becomes resistant to treatment, and this situation characterizes by treatment failing with two antipsychotic drugs for at least six weeks. Even in some cases, up to 30% of schizophrenia patients poorly responded to psychiatric medications, and about 7% have no response at all [2]. Among the methods used to treat cognitive and mental disorders is teaching math and improving learning skills. Mathematic solving skills can improve attention, self-efficacy, and memory disorders. Mathematics reduces cognitive problems by activating and developing individuals’ cognitive domains and controlling emotional and behavioral behaviors [13, 14, 15]. Therefore, considering the importance of literacy in solving the daily problems and social needs of schizophrenic patients and their possible impact on their positive and negative symptoms, and given that no study has been performed in this area, we decided to determine the effect of reading, writing, and mathematics education on the mental status of schizophrenic patients.
2. Materials and Methods
This double-blind clinical trial study was performed on patients with schizophrenia admitted to Sina Junqan Hospital (located in Chaharmahal and Bakhtiari Province in southwestern Iran) in 2015. The samples were recruited by a simple sampling method. The sample size was estimated at 30, with a 95% confidence level, and 80% power using the following formula. So there are 30 patients in the control and intervention groups, and a total of 60 samples in this study participated.
Patients were randomly divided into two groups: patients under routine treatment (control group) and patients under routine treatment with educational intervention (intervention group). Initially, there were 30 participants in each control and intervention group, but eventually, 24 patients remained in the control group and 23 in the intervention group (Figure 1). The inclusion criteria were as follows: a record of hospitalization, 15-60 years old, ability to write (lacking specific physical disabilities), no mental retardation, not being in the acute phase of illness, understanding Persian language, no visual impairment, head injury, Alzheimer disease, and addiction. Illness, addiction, and unwillingness to continue the study were considered the exclusion criteria. Eligible individuals were selected based on their educational status, positive and negative symptoms. The subjects with similar status were identified for the mentioned parameters and were randomly divided into control and intervention groups. The study data were collected using a demographic information checklist (including age, gender, education level), Anderson’s positive and negative symptoms questionnaire, and the mini-mental state examination.
Anderson’s positive and negative symptoms questionnaire is a standard instrument used in various studies in Iran. The positive symptoms section includes hallucination, delusion, bizarre behavior, and thought disorders. The choices to answer the items are non-suspicious with a score of 0-1, mild to moderate with a score of 2-3, and severe to the extreme with a score of 4-5. Higher scores indicate more severe symptoms in the respondent. The negative symptoms include affective blunting, alogia, avolition, anhedonia, social indifference, and inattention. They are rated on the same scale of positive symptoms [16, 17]. In a study in Iran, Ghamari Givi et al. reported the Cronbach α value of 0.78 for the questionnaire, and its validity was reported acceptable by exploratory factor analysis [18]. In the study of Khalaf Beigi et al., the Cronbach α value was obtained 0.78 for the negative symptoms and 0.77 for the positive symptoms [16].
The Mini-Mental State Examination (MMSE) questionnaire measures mental status. It has been translated into Persian and measures a person’s cognitive functions, including orientation, registration, attention and calculation, recent memory, and various language functions. This questionnaire has been translated into Persian and includes 19 items in various fields that measure cognitive status, with minimum and maximum possible scores of 0 to 30, respectively. Scores 25-30 indicate normal cognitive status, 20-24 possible cognitive impairment, and >19 indicate definite cognitive impairment [19]. The MMSE has also been used in Iran. For example, Seyedian et al. showed the acceptable validity and reliability of the instrument and reported the Cronbach α coefficient of 0.81 for the whole test [20].
In the intervention group, reading, writing, and math skills were taught simultaneously. Group sessions were conducted by a trained person for a maximum of 1 hour, three sessions per week. Group meetings included six to eight patients. These sessions lasted for 6 months, and at the completion of the third month, positive and negative symptoms questionnaire and the MMSE were administered to patients. During the class, the patients were categorized, and the content of the courses was selected based on a preliminary examination of patients who had previously been identified.
Because of the importance of communication for these patients, in the reading skills sessions, the trainer presented frequently used words and keywords to communicate, social conversations, meeting of social needs, and also a review of the alphabet at the beginning of the session. After ensuring learning of the vocabulary in the form of textbooks in preschool and elementary school, if patients were to progress academically, their reading comprehension skills would be reviewed. In the math lesson, after getting acquainted with the concept of numbers and related items based on preschool and first-grade content, special skills of problem-solving related to social life skills such as shopping, giving money, keeping time, and calculating distance were also taught. As with group meetings, at the beginning of each session, a review of the previous sessions and then at the end, a summary and review of the new lesson was accomplished. In addition, some exams were administered every two weeks.
After each session, the patients were given assignments for subsequent sessions. The class style was in the form of a purposeful group led by the teacher and the patients’ participation.
In addition to the beginning of the course, at the completion of the 6 months intervention, the positive and negative symptoms questionnaire and patients’ cognitive status were retested. It should be noted that at the beginning of the first class session, the class regulations were explained to the participants. In the control group, patients received routine treatments and did not undergo training. During treatment, the patients were kept as similar as possible in terms of treatment conditions, such as medication and psychology. In addition to the textbooks mentioned, some contents were determined for training in the last month by the research team and the cooperation of psychologists and physicians. These contents were taught to the patients. In addition, patients were given information about the disease, treatment, follow-up, and related issues throughout this month (by a fellow psychologist).
To strengthen the appropriate behaviors of patients during the class and in addition to their academic progress, positive reinforcement was done by giving prizes throughout the course.
The obtained data were analyzed in SPSS18 using descriptive statistics of central and dispersion indexes (mean and standard deviation) and inferential statistics of the Kolmogorov-Smirnov test and repeated measures Analyses of Variance (ANOVA). In addition, the non-parametric Mann-Whitney test was performed with a significance level of P <0.05 due to the non-normal distribution of samples.
3. Results
In this study, 47 patients with schizophrenia were assigned into two groups of 24 controls (routine therapies) and 23 cases (reading, writing, and math education and routine therapies). The Kolmogorov-Smirnov test showed that the data were normally distributed. Two groups did not show a statistically significant differences regarding age (P=0.26), gender (P=0.059), and the education level (P=0.1). Most samples in both groups had elementary education. In general, the two groups were matched in terms of age, sex, and level of education (Table 1).
.jpg)
In the two groups, the scores of positive and negative symptoms and their dimensions and MMSE in 3 stages of the study, i.e., the first time (before the intervention), second time (third months after the intervention), and third time (sixth months after the intervention) are shown in Tables 2 and 3.
.jpg)
.jpg)
In this study, the overall score of positive symptoms (P=0.038), hallucinations (P=0.033), delusions (P=0.023), and formal positive mental disorder (P=0.029) in the third time in the intervention group was significantly lower than the control group (Table 2). Also, in the case of negative symptoms, in the third time measurement, the affective blunting in the intervention group was significantly lower than the control group (P=0.039). The MMSE scores were reported for the third time in the intervention group, which were more and better than the control group (P=0.013).
Based on the findings of repeated measures AVOVA, changes in the overall score of positive symptoms and all its dimensions were statistically significant and decreased in the intervention group (P<0.001), but in the control group, only changes in positive thought disorder (P=0.031) and bizarre behaviors (P<0.001) were significant. Regarding the changes in the score of the first and third month of positive symptoms, the findings showed that the difference between the score of the first and third times in the total score of positive symptoms and all its dimensions is significantly different between the two groups (P<0.05) (Table 2).
Based on the findings of repeated measures ANOVA, changes in the overall score of negative symptoms and all its dimensions were statistically significant and decreased in the intervention group (P<0.001), except for alogia compared to the control group (P=0.124). The rest of the dimensions were significant. Also, the MMSE was reported in both control and intervention groups (P<0.05). Regarding negative symptoms, there is a significant difference between the two groups in the scores of the first and third times in the overall score of negative symptoms and some of its dimensions, including affective blunting and alogia (P<0.05). The difference between the scores of the first and third times of the short mental status test was also reported significant between the two groups (P<0.05) (Tables 2 and 3).
Changes in the MMSE score also were significant in both intervention (P=0.002) and control (P=0.017) groups, but in comparison between the two groups, this rate was higher in the intervention group after the sixth month (Table 4).

4. Discussion
The current study was conducted to investigate the effect of reading, writing, and math education on the mental state of schizophrenic patients. In this study, the overall scores of positive symptoms, hallucinations, delusions, and formal positive thought disorder were lower in the third time (After six months of intervention) measurement in the intervention group compared to that in the control group. In the case of negative symptoms, in the third measurement, the affective blunting was significantly lower in the intervention group than in the control group. The standard schizophrenia treatment based on biological, psychological, and social models includes the administration of antipsychotic drugs, psychological interventions, and social and family support [21]. In general, there is extensive evidence of the effectiveness of life skills training on social, cognitive, and emotional functioning in patients with schizophrenia [22].
Research has shown that life skills training, including social skills, is associated with improved patient cognitive function, especially in terms of verbal ability, information processing speed, and memory.
Some research has shown that these kinds of training increase problem-solving skills, the quality of conversational skills, cognitive interactions, positive symptoms, long-term visual memory, self-expression, and communication with others while reducing relapse periods [22, 23, 24, 25]. On the other hand, reading, writing, and math training are cognitive in nature, which is related to their effect on the psychological symptoms of patients with schizophrenia. One study showed that poetry, storytelling, and other texts had a great impact on improving patient interactions, reducing impulsivity, increasing realism, improving self-care, interpersonal relationships, and increasing patient participation [26].
In their study of 82 patients with schizophrenia, Aubin et al. found significant relationships between performance and visual-spatial learning, spatial memory, and negative symptoms in patients with schizophrenia [27]. A study by Steel et al. showed that positive memory training protocol was an effective, inexpensive, and convenient method, and because the dominant focus of the intervention was on past positive experiences, the patient’s involvement would be high [28].
In the current study, the changes in the MMSE score were significant in both the intervention and control groups. In the third time (6 months after the intervention), the scores were higher in the intervention group. Greiq et al. conducted a one-year study of neuro-cognitive therapy to identify cognitive impairments in patients with schizophrenia who had participated in an occupational therapy program. That study included computer cognitive training exercises. One year after treatment, patients receiving neurological and occupational therapy showed significant improvements in executive functions and working memory compared to patients who had only undergone occupational therapy [29]. A review study also showed that science learning and memory enhancement could potentially enhance cognitive function, increase attention, increase drug effectiveness, and reduce symptoms and duration of illness in people with schizophrenia [30]. For other neuropsychiatric disorders, studies have also been conducted on the effectiveness of teaching skills, such as reading and writing, and math. In this regard, a study was conducted to teach basic concepts and strengthen the ability to read and write on the patient undergoing the intervention. Statistical analysis showed that the intervention group attained sufficient skills of reading and writing, and the cognitive intervention improved cognitive function in the intervention group [31]. Another study also showed that reading, writing, math, and content interventions improve the behavioral and academic outcomes of students with emotional and behavioral disorders. This training had positive outcomes for students’ symptoms and academic achievement and improved their cognitive processes [32]. Thus, schizophrenia, which is often associated with cognitive impairment such as objective thinking, information processing disorder, impaired social and occupational activity, impaired social cognition, impaired interpersonal relationships, and low responsibility, can be partially addressed by teaching a variety of life skills to reduce existing deficiencies. Teaching these skills helps the patient to cope with the positive symptoms of their illnesses through acquiring the self-management skills of the negative symptoms learning how to communicate verbally and non-verbally with others, and making appropriate emotional statements. Eventually, the patients will be able to partly control social anxiety and avoidance behaviors by learning how to communicate with others in different situations (through role-playing and role modeling).
Therefore, learning social and life skills has led to the patients’ self-help and their active participation in controlling the symptoms of illness and the development of self-management skills. In this way, the patients gain better insight into their condition, leading to greater acceptance of responsibility for their behaviors [33].
Learning to read and write and math exercises can be effective in improving the positive and negative symptoms of patients with schizophrenia and improving their cognitive symptoms.
However, it is recommended that these methods be used in addition to conventional therapies to improve patients’ cognitive status as a complementary treatment in the health and rehabilitation centers. It is recommended that future studies be conducted with larger sample size and compare this treatment with other types of cognitive therapies.
Ethical Considerations
Compliance with ethical guidelines
This study was approved by the Ethics Committee of the Shahrekord University of Medical Sciences (Code: IR.SKUMS.REC.91-5-4).
Funding
This study was extracted from a research project approved by the Deputy of Research and Technology of Shahrekord University of Medical Sciences (No. 1150).
Authors' contributions
Study design, and writing of the manuscript: Masoud Nikfarjam and Najmeh Khosravi; Data collection: Neda Parvin; Data analysis and initial review: Forouzan Ganji; Preparation and final approval of manuscript: Iraj Goodarzi, Abdollah Mohammadi-ahmadmahmoudi, Masoud Nikfarjam, Najmeh Khosravi, Forouzan Ganji, and Neda Parvin.
Conflicts of interest
The authors declared no conflict of interest.
Refrences
- Charlson FJ, Ferrari AJ, Santomauro DF, Diminic S, Stockings E, Scott JG, et al. Global epidemiology and burden of schizophrenia: Findings from the global burden of disease study 2016. Schizophrenia Bulletin. 2018; 44(6):1195-203. [DOI:10.1093/schbul/sby058] [PMID] [PMCID]
- Birnbaum ML, Wan CR, Broussard B, Compton MT. Associations between duration of untreated psychosis and domains of positive and negative symptoms. Early Intervention in Psychiatry. 2017; 11(5):375-82. [DOI:10.1111/eip.12256]
- Reichenberg A. The assessment of neuropsychological functioning in schizophrenia. Dialogues in Clinical Neuroscience. 2010; 12(3):383-92. [DOI:10.31887/DCNS.2010.12.3/areichenberg] [PMID] [PMCID]
- Khan ZU, Martin-Montañez E, Muly EC. Schizophrenia: Causes and treatments. Current Pharmaceutical Design. 2013; 19(36):6451-61. [DOI:10.2174/1381612811319360006][PMID
- Picchioni MM, Murray RM. Schizophrenia.The BMJ. 2007; 335(7610):91-5. [DOI:10.1136/bmj.39227.616447.BE] [PMID] [PMCID]
- Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016; 388(10039):86-97. [DOI:10.1016/S0140-6736(15)01121-6] [PMID] [PMCID]
- Stępnicki P, Kondej M, Kaczor AA. Current concepts and treatments of schizophrenia. Molecules. 2018; 23(8):2087. [DOI:10.3390/molecules23082087] [PMID] [PMCID]
- Staiger T, Waldmann T, Rüsch N, Krumm S. Barriers and facilitators of help-seeking among unemployed persons with mental health problems: A qualitative study. BMC Health Services Research. 2017; 17(1):39. [DOI:10.1186/s12913-017-1997-6] [PMID] [PMCID]
- Guarnera M, Pellerone M, Commodari E, Valenti GD, Buccheri SL. Mental images and school learning: A longitudinal study on children. Frontiers in Psychology. 2019; 10:2034. [DOI:10.3389/fpsyg.2019.02034] [PMID] [PMCID]
- Harvey AG, Lee J, Williams J, Hollon SD, Walker MP, Thompson MA, et al. Improving outcome of psychosocial treatments by enhancing memory and learning. Perspectives on Psychological Science. 2014; 9(2):161-79. [DOI:10.1177/1745691614521781] [PMID] [PMCID]
- Lyon AR, Stirman SW, Kerns SE, Bruns EJ. Developing the mental health workforce: Review and application of training approaches from multiple disciplines. Administration and Policy in Mental Health. 2011; 38(4):238-53. [DOI:10.1007/s10488-010-0331-y] [PMID] [PMCID]
- Revheim N, Corcoran CM, Dias E, Hellmann E, Martinez A, Butler PD, et al. Reading deficits in schizophrenia and individuals at high clinical risk: Relationship to sensory function, course of illness, and psychosocial outcome. Amreican Journal of Psychiatry. 2014; 171(9):949-59. [DOI:10.1176/appi.ajp.2014.13091196] [PMID] [PMCID]
- Bigdeli IA, Mohammadifar MA, Rezaei A, AbdolHoseinzadeh A. [The effect of mathematic problem – solving training with playing – based method on attention, problem – solving and self – efficacy in student with mathematic learning disability (Persian)]. Research in School and Virtual Learning. 1970; 4(14):41-52. http://etl.journals.pnu.ac.ir/article_3168.html?lang=en
- Kroesbergen EH, Van Luit JEH. Constructivist mathematics education for students with mild mental retardation. European Journal of Special Needs Education. 2005; 20(1):107-16. [DOI:10.1080/0885625042000319115]
- Passolunghi MC, Vercelloni B, Schadee H. The precursors of mathematics learning: Working memory, phonological ability and numerical competence. Cognitive Development. 2007; 22(2):165-84. [DOI:10.1016/j.cogdev.2006.09.001]
- Khalafbaigi M, Bayanzadeh A, Zadeh-mohammadi A, Shafaroodi N. [The effect of musical activity on memory and attention in schizophrenia (Persian)]. Journal Iran of Psychiatry & Clinical Psychology. 2006; 12(3):236-43. http://ijpcp.iums.ac.ir/article-1-8-en.htm
- Froozandeh N, akbari N, Kazemian A, hasanpoor A, safdari F, froozandeh M. [The effect of occupational therapy on positive and negative symptoms in schizophrenic patients (Persian)]. Journal of Shahrekord University of Medical Sciences. 2007; 9(3):21-27. http://78.39.35.44/article-1-422-en.html
- Ghamari Givi H, Moulavi P, Heshmati R. [Exploration of the factor structure of positive and negative syndrome scale in schizophernia spectrum disorder (Persian)]. Journal of Clinical Psychology. 2010; 2(2):1-10. [DOI:10.22075/jcp.2017.2018] https://jcp.semnan.ac.ir/article_2018.html?lang=en
- Schröder J, Niethammer R, Geider FJ, Reitz C, Binkert M, Jauss M, et al. Neurological soft signs in schizophrenia. Schizophrenia Research. 1991; 6(1):25-30. [DOI:10.1016/0920-9964(91)90017-l] [PMID]
- Seyedian M, Fallah M, Noroozian M NS, Delavar A, H Gz. Designing and determination of the validity of the Persian version of Mini-Mental State Examination. J Med Counc Islam Repub Iran. 2007; 25(4):408-14. http://jmciri.ir/browse.php?a_id=1170&sid=1&slc_lang=fa
- Rahmati M, Fallahi Khoshknab M, rahgou A, rahgozar M. [The effect of spiritual-religious group therapy on mental status of schizophrenic inpatients (Persian)]. Iranian Journal of Nursing Research. 2010; 5(16):13-20. http://ijnr.ir/article-1-586-en.html
- Turner DT, McGlanaghy E, Cuijpers P, van der Gaag M, Karyotaki E, MacBeth A. A meta-analysis of social skills training and related interventions for psychosis. Schizophrenia Bulletin. 2018; 44(3):475-91. [DOI:10.1093/schbul/sbx146] [PMID] [PMCID]
- Horan WP, Kern RS, Tripp C, Hellemann G, Wynn JK, Bell M, et al. Efficacy and specificity of social cognitive skills training for outpatients with psychotic disorders. Journal of Psychiatric Research. 2011; 45(8):1113-22. [DOI:10.1016/j.jpsychires.2011.01.015] [PMID] [PMCID]
- Yildiz M, Özaslan Z, İncedere A, Kircali A, Kiras F, İpçi K. The effect of psychosocial skills training and metacognitive training on social and cognitive functioning in schizophrenia. NoroPsikiyatri Arsivi. 2018; 56(2):139-43. [DOI:10.29399/npa.23095] [PMID] [PMCID]
- Pontes LM, Martins CB, Napolitano IC, Fonseca JR, Oliveira GM, Iso SM, et al. Cognitive training for schizophrenia in developing countries: A pilot trial in Brazil. Schizophrenia Research Treatment. 2013; 2013:321725. [DOI:10.1155/2013/321725] [PMID] [PMCID]
- Golden KM. The use of collaborative writing to enhance cohesion in poetry therapy groups. Journal of Poetry Therapy. 2000; 13(3):125-38. [DOI:10.1023/A:1021473712505]
- Aubin G, Stip E, Gélinas I, Rainville C, Chapparo C. Daily activities, cognition and community functioning in persons with schizophrenia. Schizophrenia Research. 2009; 107(2-3):313-8. [DOI:10.1016/j.schres.2008.08.002] [PMID]
- Steel C, van der Gaag M, Korrelboom K, Simon J, Phiri P, Baksh MF, et al. A randomised controlled trial of positive memory training for the treatment of depression within schizophrenia. BMC Psychiatry. 2015; 15:85. [DOI:10.1186/s12888-015-0453-6] [PMID] [PMCID]
- Greig TC, Zito W, Wexler BE, Fiszdon J, Bell MD. Improved cognitive function in schizophrenia after one year of cognitive training and vocational services. Schizophrenia Research. 2007; 96(1-3):156-61. [DOI:10.1016/j.schres.2007.07.003] [PMID] [PMCID]
- Lawlor-Savage L, Goghari VM. Working memory training in schizophrenia and healthy populations. Behavioral Science. 2014; 4(3):301-19. [DOI:10.3390/bs4030301] [PMID] [PMCID]
- Fabio RA, Castelli I, Marchetti A, Antonietti A. Training communication abilities in rett syndrome through reading and writing. Frontiers in Psychology. 2013; 4:911. [DOI:10.3389/fpsyg.2013.00911] [PMID] [PMCID]
- Campbell AR, Bowman-Perrott L, Burke MD, Sallese MR. Reading, writing, math, and content-area interventions for improving behavioral and academic outcomes of students with emotional and behavioral disorders. Learning Disabilities: A Contemporary Journal. 2018; 16(2):119-38. https://eric.ed.gov/?id=EJ1194543
- Almerie MQ, Okba Al Marhi M, Jawoosh M, Alsabbagh M, Matar HE, Maayan N, et al. Social skills programmes for schizophrenia. Cochrane Database Systematic Reviews. 2015; 2015(6):CD009006. [DOI:10.1002/14651858.CD009006.pub2] [PMID] [PMCID]
Type of Study: Original |
Subject:
Mental Health
Received: 2020/11/2 | Accepted: 2021/07/7 | Published: 2021/10/1
Received: 2020/11/2 | Accepted: 2021/07/7 | Published: 2021/10/1
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |


.jpg)